What is
Leukemia:
 From
the Greek meaning "white blood". Leukemia is a
cancer of a
marrow cell. The term refers to a group of closely related malignant conditions
affecting the immature blood-forming cells in the bone marrow. so is that
certain cells in the body become abnormal. Another is that the body keeps
producing large numbers of white cells. From
the Greek meaning "white blood". Leukemia is a
cancer of a
marrow cell. The term refers to a group of closely related malignant conditions
affecting the immature blood-forming cells in the bone marrow. so is that
certain cells in the body become abnormal. Another is that the body keeps
producing large numbers of white cells.
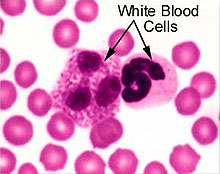
Under normal circumstances, cells are formed, mature, carry out their function,
and die. New cells are constantly being formed to take their places. Normal
blood contains 3 major groups of cells: white blood cells, red blood cells, and
platelets. All 3 types develop from one immature cell type called stem cells in
a process called hematopoiesis.
|
In humans, the bones are not
solid, but are made up of two distinct regions. The outer,
weight-bearing area is hard, compact, and calcium-based. It surrounds a
lattice-work of fibrous bone known as cancellous tissue. The inner
region, or marrow - which is one of the largest organs of the body - is
located within the bones.
The marrow may contain fat cells,
fluid, fibrous tissue, blood vessels, and hematopoietic, or blood-forming,
cells. Marrow looks yellow when it holds many fat cells; it appears red when
it has more blood-forming material. The marrow is the principal site for
hematopoiesis (blood formation), which, after birth, occurs primarily within
the bones of the legs, arms, ribs, sternum (breastbone), and vertebrae
(backbones).

|
Leukemia occurs when immature or mature
cells multiply in an uncontrolled manner in the bone marrow. It is classified as
lymphocytic or myeloid, according to the type of cell that is multiplying
abnormally, and either acute, signifying rapidly progressing disease with a
predominance of highly immature (blastic) cells, or chronic, which denotes
slowly progressing disease with greater numbers of more mature cells
What Causes Leukemia:
The exact cause of most cases of
leukemia is not known. But doctors have found that this cancer is linked to a
number of risk factors.
-
 Smoking
is considered a risk factor for leukemia, as for other cancers, but many
people who have leukemia never smoked, and many people who smoke never get
leukemia. Potential leukemia-causing chemicals in tobacco smoke include
benzene, polonium-210, and polycyclic aromatic hydrocarbons (PAHs). These
carcinogens (cancer-causing substances) are absorbed by the lungs and are
spread via the bloodstream. It is estimated that one in four cases of
acute myelogenous leukemia (AML)
is the result of cigarette smoking. Smoking
is considered a risk factor for leukemia, as for other cancers, but many
people who have leukemia never smoked, and many people who smoke never get
leukemia. Potential leukemia-causing chemicals in tobacco smoke include
benzene, polonium-210, and polycyclic aromatic hydrocarbons (PAHs). These
carcinogens (cancer-causing substances) are absorbed by the lungs and are
spread via the bloodstream. It is estimated that one in four cases of
acute myelogenous leukemia (AML)
is the result of cigarette smoking.
-
Long-term exposure to chemicals such as benzene or formaldehyde, typically
in the workplace, is considered a risk factor for leukemia, but this
accounts for relatively few cases of the disease.
-
Exposure to extraordinarily high
doses of radiation is a risk factor, although this accounts for
relatively few cases of leukemia. It is important to note, however, that
standard diagnostic X-rays pose little or no increase in leukemia risk.
Other risk factors for leukemia
include the following:
-
Previous
chemotherapy: Drugs called alkylating agents used to treatment certain
types of cancers are linked to development of leukemia later.
Acute myelogenous leukemia (AML) has been reported after chemotherapy
and/or radiotherapy for various solid tumors (breast
cancer,
ovarian cancer),
blood malignancies, and nonmalignant conditions. The chemotherapeutic agents
most often associated with secondary leukemias are procarbazine,
chlorambucil, etoposide, mechlorethamine, teniposide, and cyclophosphamide.
The risk is increased when these drugs are combined with radiation therapy.
-
Human T-cell leukemia virus 1
(HTLV-1): Infection with this virus is linked to human T-cell leukemia.
Excess leukemias also have been reported in workers who are exposed to
animal viruses - for example, butchers, slaughterhouse workers, and
veterinary practitioners.
-
Myelodysplastic syndrome: This blood disorder increases the risk of acute
myelogenous leukemia.
-
 Down
syndrome and other genetic diseases: Leukemia risk is increased 15-fold
among children with Down's syndrome, which is a genetically linked
chromosomal abnormality (usually an extra copy of chromosome 21). Three rare
inherited disorders - Fanconi's anemia, Bloom's syndrome, and ataxia
telangiectasia - also have a greatly increased risk of leukemia. In
addition, leukemia varies among racial and ethnic groups with different
genetic make-ups. Down
syndrome and other genetic diseases: Leukemia risk is increased 15-fold
among children with Down's syndrome, which is a genetically linked
chromosomal abnormality (usually an extra copy of chromosome 21). Three rare
inherited disorders - Fanconi's anemia, Bloom's syndrome, and ataxia
telangiectasia - also have a greatly increased risk of leukemia. In
addition, leukemia varies among racial and ethnic groups with different
genetic make-ups.
-
Family history: Having a
first-degree relative who has chronic lymphocytic leukemia increases your
risk of having the disease by as much as 4 times that of someone who does
not have an affected relative.
-
Age - Roughly 60% to 70% of leukemias occur in people who are older
than 50.
Translocations are another type of DNA problem that can lead to leukemia.
Human DNA is packaged in 23 pairs of chromosomes. If DNA from one chromosome
gets attached to the wrong chromosome, cancer can result.
Types of Leukemia:
 Bone
marrow, the material filling the body's bones, is the adult source of the body's
blood cells and produces two blood cell lines, the myeloid and the
lymphoid. Bone
marrow, the material filling the body's bones, is the adult source of the body's
blood cells and produces two blood cell lines, the myeloid and the
lymphoid.
Myeloid Cell Line. The myeloid cell line includes early cells that
mature into red
blood cells, blood clotting agents (platelets), and some white blood
cells. These white blood cells include
macrophages,
eosinophils, and
neutrophils.
Lymphoid Cell Line. The lymphoid cell line includes two of the
body's primary infection fighters known as T-cell and B-cell
lymphocytes
. Part of their role is to produce antibodies, factors that can target and
attack specific foreign agents (antigens) in the body.
Depending on the types of cell the
disease appears in one of four major forms:
-
 Acute
lymphocytic leukemia- Acute lymphocytic leukemia, also called
acute lymphoblastic leukemia and acute lymphoid leukemia, is a common
leukemia. About 4,000 new cases are diagnosed each year in the United
States. Most cases of acute lymphocytic leukemia (ALL) occur in children
under age 10, but it can appear in all age groups. ALL is an acute leukemia,
which means it is a disease that gets worse quickly. Acute
lymphocytic leukemia- Acute lymphocytic leukemia, also called
acute lymphoblastic leukemia and acute lymphoid leukemia, is a common
leukemia. About 4,000 new cases are diagnosed each year in the United
States. Most cases of acute lymphocytic leukemia (ALL) occur in children
under age 10, but it can appear in all age groups. ALL is an acute leukemia,
which means it is a disease that gets worse quickly.
-
Acute myelogenous leukemia characterized by the
uncontrolled proliferation and accumulation of abnormal immature cells,
referred to as leukemic blasts. These cells fill the marrow spaces and enter
the blood.
-
Chronic myelogenous leukemia - Chronic myelogenous
leukemia (CML) is a myeloproliferative disorder characterized by increased
proliferation of the granulocytic cell line without the loss of their
capacity to differentiate, and
-
Chronic lymphocytic leukemia are less rapidly
progressive.
The former, however, requires treatment
in nearly all cases at the time of diagnosis, whereas the later may, in some
cases, be non-progressive for long periods
Symptoms of Leukemia:
Broad
symptoms of leukemia may include:
-
 Fatigue Fatigue
-
Malaise (vague feeling of bodily
discomfort)
-
Abnormal bleeding
-
Excessive bruising
-
Weakness
-
Reduced exercise tolerance
-
Weight loss
-
Bone or joint pain
-
Infection and fever
-
Abdominal pain or "fullness"
-
Enlarged spleen, lymph nodes, and
liver
-
Chronic leukemia often goes undetected
for many years until it is identified in a routine blood test. In fact,
nearly one in five chronic leukemia patients have no symptoms at the time of
their diagnosis. Most symptoms of acute leukemia are caused by a lack of
normal blood cells. This is due to overcrowding of the blood-forming bone
marrow by leukemia cells.
Signs of Blood Abnormalities
Once the patient's blood is tested, signs of specific blood abnormalities may be
noted, such as:
-
Anemia - a low number of erythrocytes (red blood cells) within the
blood. Anemia can cause fatigue, "pale" skin coloration, and respiratory
difficulties such as shortness of breath.
-
Leukopenia - a low number of normal
leukocytes (white blood cells) that may increase the risk of infection. A
reduction in WBC count is also encountered with toxemia and septicemia.
-
Neutropenia (granulocytopenia) - too
few mature neutrophils, the mature bacteria-destroying white blood cells
that contain small particles, or granules.
-
Thrombocytopenia - a low number of
blood-clotting platelets that can result in excessive bruising, abnormal
bleeding, or frequent bleeding of the nose or gums.
-
Thrombocytosis - a high number of
platelets. Some patients, especially those with chronic myelogenous leukemia
(CML), may exhibit thrombocytosis, although their platelets may not clot
properly, causing bruising and bleeding difficulties.
-
 Because
leukemia may cause enlarged spleen (splenomegaly) and enlarged liver
hepatomegaly (enlarged liver), the overgrowth of these organs may appear as
belly "fullness" or swelling. Such fullness may be palpated (felt) by the
physician during physical examination. Lymph node enlargement may or may not
be apparent, although imaging studies should be able to confirm any
lymphatic disease. Because
leukemia may cause enlarged spleen (splenomegaly) and enlarged liver
hepatomegaly (enlarged liver), the overgrowth of these organs may appear as
belly "fullness" or swelling. Such fullness may be palpated (felt) by the
physician during physical examination. Lymph node enlargement may or may not
be apparent, although imaging studies should be able to confirm any
lymphatic disease.
-
Leukemia that has spread to the brain
may produce central nervous system effects, such as headaches, seizures,
weakness, blurred vision, balance difficulties, or vomiting.
Certain forms of leukemia produce more
distinct symptoms. For example,
acute myelogenous leukemia (AML),
particularly the M5 monocytic form, may generate tell-tale symptoms such as:
-
swollen, painful, and bleeding gums -
if AML has spread to the oral tissue;
-
pigmented (colored) rash-like spots -
if AML has spread to the skin; or
-
chloromas - if AML has spread to the skin or other organs.
The T-cell variety of
acute lymphocytic leukemia (ALL)
may cause the thymus to enlarge and press on the trachea (windpipe). Such
pressure may lead to:
-
shortness of breath,
-
coughing, or
-
suffocation.
If the overgrown thymus presses upon the
superior vena cava (SVC), the large vein that carries blood from the head and
arms back to the heart, this may produce
SVC syndrome. SVC involvement of the brain can be fatal.
Diagnosis of Leukemia:
The following methods may be used to
diagnose leukemia:
-
The signs and symptoms may suggest a
diagnosis of leukaemia. On examination there may be enlarged lymph glands,
hepatomegaly and/or
splenomegaly.
-
A urine sample is checked for blood.
-
Blood tests such as a full blood count
will check the number of each type of white blood cell in the sample. It will
indicate the presence of anaemia or a reduction in the number of platelets.
-
A blood film is done to check the
appearance of the blood cells. This involves taking a very small amount of blood
from the sample and smearing it on a slide, which is then viewed under a
microscope. Immature or abnormal blood cells can be seen on the slide.
-
 Bone
marrow biopsy involves the removal of some bone and marrow from the sternum or
the hipbone. This is usually done under local anaesthetic, although in small
children general anaesthetic may be required. The sample of bone marrow is
spread on a slide and examined under a microscope. Bone
marrow biopsy involves the removal of some bone and marrow from the sternum or
the hipbone. This is usually done under local anaesthetic, although in small
children general anaesthetic may be required. The sample of bone marrow is
spread on a slide and examined under a microscope.

A beam of light (usually laser light) of a single frequency (colour) is directed
onto a hydrodynamically focused stream of fluid. A pair of detectors are aimed
at the point where the stream passes through the light beam; one in line with
the light beam and one perpendicular to it. Each suspended particle passing
through the beam scatters the light in some way, and chemicals in the particle
may be excited into emitting light at a lower frequency than the light source.
This combination of scattered and fluorescent light is picked up by the two
detectors, and by analyzing fluctuations in brightness and frequency at each
detector it is possible to deduce various facts about the physical and chemical
structure of each individual particle.
Treatment of Leukemia:
 Chemotherapy,
radiotherapy and bone marrow transplant (BMT) are used to treat
leukaemia. There are different types of chemotherapy (called protocols) each
involving a number of anticancer drugs given at the same time. Chemotherapy,
radiotherapy and bone marrow transplant (BMT) are used to treat
leukaemia. There are different types of chemotherapy (called protocols) each
involving a number of anticancer drugs given at the same time.
The effectiveness of treatment for
leukaemia depends on the type and stage of the disease. Acute leukaemia often
goes into
remission. However, many people with acute leukaemia have a relapse (the
disease returns).
Chronic leukaemias develop more slowly than the acute types, but respond less
well to chemotherapy and are rarely cured.
Acute leukaemia
Acute leukaemia is treated with
chemotherapy to destroy the abnormal cancer cells. Mixtures of drugs are given
into a vein in a series of treatment courses.
Medicines are available which reduce the
side-effects of chemotherapy such as nausea. Hair may fall out during treatment
but it re-grows once the chemotherapy has stopped. Some people may be able to
use "cold caps" which cool the scalp and help prevent hair loss.
If the leukaemia returns (relapses),
intensive treatment may be given. This involves a bone marrow or a stem cell
transplant. Bone marrow or stem cell transplants allow much higher doses of
chemotherapy to be given.
Before transplantation, very high doses
of chemotherapy and sometimes radiotherapy are given to destroy all the bone
marrow, both abnormal and normal. This improves the chance of completely curing
the leukaemia.
Then normal bone marrow cells, donated
from a close relative or carefully removed from the person's own bone marrow,
are infused into the bloodstream with a drip.
Stem cell transplant involves
transplanting
stem cells, rather than bone marrow cells. Stem cells can be harvested
(collected) from a leukaemia patient's own blood or from a donor. New
alternatives, which are currently experimental, include harvesting stem cells
from umbilical cord blood or placentas of new born babies.
|
SKIN-TUNNELED CATHETER
 A
skin-tunneled catheter is a flexible plastic tube passed through the
skin of the chest and inserted into the subclavian vein, which leads to
the heart. It is often used in people who have leukaemia or other
cancers and need to have regular
chemotherapy and
blood tests. Using the catheter, drugs can be injected directly
into the bloodstream and blood samples can be obtained easily. A
skin-tunneled catheter is a flexible plastic tube passed through the
skin of the chest and inserted into the subclavian vein, which leads to
the heart. It is often used in people who have leukaemia or other
cancers and need to have regular
chemotherapy and
blood tests. Using the catheter, drugs can be injected directly
into the bloodstream and blood samples can be obtained easily.
The catheter is inserted under local
anaesthesia and can remain in position for months. The external end is
plugged when not in use. Because the catheter is inserted through the skin
some distance away from the site of entry into the vein, the risk of infection
is reduced.
Using the catheter
The catheter is tunneled under the skin
and enters the subclavian vein to lie with its tip in the heart. A syringe
can be attached to inject drugs.
|
Chronic leukaemia
Treatment for chronic leukaemia depends
on its type and stage. Often treatment is not started unless there are symptoms.
In the early stage, treatment aims to control symptoms by reducing the number of
abnormal cells in the blood.
Biological therapy may be an option for
certain types of leukaemia, such as
chronic myeloid leukaemia (CML).
This involves treatment with
natural substances.
As the condition becomes more advanced,
treatment may consist of mild chemotherapy, blood transfusion and antibiotics
for infections. Some evidence indicates that in chronic myeloid leukaemia, bone
marrow transplantation can prolong life if performed during its chronic phase.
Another available treatment is
monoclonal antibodies. Antibodies are proteins that are produced by certain
cells in response to infection. They usually attach themselves to bacteria or
viruses and help to destroy them. A type of specifically manufactured monoclonal
antibody that recognizes and selectively destroys leukaemia cells can be infused
into the body. An example is alemtuzumab (MabCampath), which is used to treat
chronic lymphocytic leukaemia (CLL).
|
Bone Marrow Transplant
 The
choice of treatment and timing of BMT depends on a number of factors including
the patient's age and general health, and the type and stage of the leukaemia.
In a bone marrow transplant, cancerous or abnormal bone marrow is replaced with
healthy marrow. Before the transplant, the recipient's abnormal bone
marrow is eliminated by chemotherapy or radiotherapy. Healthy marrow may
have been supplied by a donor or by the patient when the underlying disease was
inactive. Up to 1 litre (2 pints) of bone marrow may be extracted from the
hipbone with a syringe through a hollow needle. The
choice of treatment and timing of BMT depends on a number of factors including
the patient's age and general health, and the type and stage of the leukaemia.
In a bone marrow transplant, cancerous or abnormal bone marrow is replaced with
healthy marrow. Before the transplant, the recipient's abnormal bone
marrow is eliminated by chemotherapy or radiotherapy. Healthy marrow may
have been supplied by a donor or by the patient when the underlying disease was
inactive. Up to 1 litre (2 pints) of bone marrow may be extracted from the
hipbone with a syringe through a hollow needle.
BMT may be allogenic or autologous. Allogenic BMT requires a donor, often a
relative, whose tissue type is a match for that of the patient. With autologous
BMT some of the patient's own bone marrow is removed, treated with
chemotherapeutic drugs to kill all the abnormal cells and frozen to be used
later.
With both types of BMT the patient receives high doses of chemotherapy and
radiation to destroy their bone marrow and any leukaemic cells in the body. The
donor, or autologous bone marrow, is then injected into the patient. BMT
requires specialized care and support to prevent infection or rejection of the
bone marrow.
Transplantation procedures are
difficult, and side effects are common. They include nausea, vomiting, fatigue,
mouth sores, and loss of appetite. The procedures can also be dangerous and
carry a small risk for death. One of the most serious side effects of both bone
marrow and stem cell transplants is the risk of infection, which can persist for
several months after the transplant. Pneumonia, cytomegalovirus,
aspergillus, and Pneumocystis carini I (a protozoan) are among the
most important life-threatening infections.
|
Namita Nayyar (WF Team)
Dated 19 January 2013
Related Links
|









