|
|
Cancer is a
frightening word surrounded by fears and myths. One of the greatest fears
expressed by almost all newly diagnosed cancer patients is: `Am I going to
die?'
|
Approximately
I80, 000 American women are newly diagnosed with breast cancer disease each year, and it is the
leading killer of women in midlife (ages forty to fifty� five) . The only
cancer that kills more women overall is lung cancer , but breast cancer is
actually responsible for more years of life lost because it generally
afflicts younger women. On top of the physical health problems, breast
cancer can also exert a large emotional and psychological toll, because it
affects a part of the body that many women associate directly with either
femininity. Surveys have consistently found that women perceive cancer to be
their greatest health threat.
|
|
The Breast and Breast
Cancer
Breasts are made up of several sections called lobes. Each
lobe has smaller sections called lobules, which produce milk when a woman is
breast � feeding. The lobes and lobules are linked by tubes called ducts. Ducts
are the tubes that carry the milk from the lobules to the nipple. The rest of
the breast is mostly
 made up of fat but also consists of veins, arteries,
nerves, and other tissue. Cancer is a term for disease in which abnormal
cells divide without control. Cancer cells can invade nearby tissues and spread
through the blood stream and lymphatic system to other parts of the body.
Breast cancer is a malignant tumor that has developed from cells of the breast.
A malignant tumor is a group of cancer cells that may invade surrounding
tissues or spread (metastasize) to distant areas of the body. The disease occurs
mostly in women, but men can get it, too. made up of fat but also consists of veins, arteries,
nerves, and other tissue. Cancer is a term for disease in which abnormal
cells divide without control. Cancer cells can invade nearby tissues and spread
through the blood stream and lymphatic system to other parts of the body.
Breast cancer is a malignant tumor that has developed from cells of the breast.
A malignant tumor is a group of cancer cells that may invade surrounding
tissues or spread (metastasize) to distant areas of the body. The disease occurs
mostly in women, but men can get it, too.
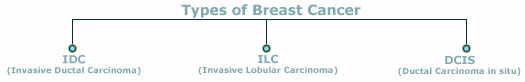
Types of Breast Cancer
In breast cancer, cells in the breast divide and grow at an
abnormal rate, clump together, and from a malignant (cancerous) tumor. There are
two main types of breast cancer.
-
Invasive Ductal Carcinoma (IDC)- This is a
cancer starts in a milk passage, or duct, of the breast, has broken
through the wall of the duct, and invaded the fatty tissue of the breast. At
this point, it can metastasize, or spread to other parts of the body through the
lymphatic system (The tissues and organs that
produce, store, and carry white blood cells that fight infections and other
diseases. This system includes the bone marrow, spleen, thymus, lymph nodes, and
lymphatic vessels (a network of thin tubes that carry lymph and white blood
cells). ) and bloodstream. About 80% of invasive breast cancers are
infiltrating ductal carcinomas.
-
Invasive Lobular Carcinoma (ILC)- Infiltrating
lobular carcinoma starts in the milk-producing glands, or lobules. Similar to
IDC, it also can spread (metastasize) to other parts of the body. About 10% of
invasive breast cancers are ILCs. Invasive lobular carcinoma may be harder to
detect by mammography than invasive ductal carcinoma. Stage 1 tumours: these measure less than two centimeters. The lymph
glands in the armpit are not affected and there are no signs that the cancer has
spread elsewhere in the body.
Stage 2 tumours: these measure between two and five centimeters, or the
lymph glands in the armpit are affected, or both. However, there are no signs
that the cancer has spread further.
Stage 3 tumours: these are larger than five centimeters and may be
attached to surrounding structures such as the muscle or skin. The lymph glands
are usually affected, but there are no signs that the cancer has spread beyond
the breast or the lymph glands in the armpit.
Stage 4 tumours: these are of any size, but the lymph glands are usually
affected and the cancer has spread to other parts of the body. This is secondary
breast cancer.
-
Ductal Carcinoma in situ (DCIS) - This is also called
a noninvasive breast cancer,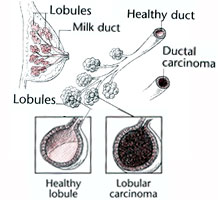 where
there are abnormal cells in the breast, but they are not cancerous and have not
spread to other nearby tissue. In situ means �in place�. Still, carcinoma in
situ is a sign that breast cancer may develop at a latter time. The main
categories of carcinoma in situ are ductal carcinoma in situ (DCIS) �where the
abnormal cells originate in the milk ducts � and lobular carcinoma in situ (LCIS)
� where the abnormal cells originate in the lobules. A mammogram is the best way
to find DCIS early. where
there are abnormal cells in the breast, but they are not cancerous and have not
spread to other nearby tissue. In situ means �in place�. Still, carcinoma in
situ is a sign that breast cancer may develop at a latter time. The main
categories of carcinoma in situ are ductal carcinoma in situ (DCIS) �where the
abnormal cells originate in the milk ducts � and lobular carcinoma in situ (LCIS)
� where the abnormal cells originate in the lobules. A mammogram is the best way
to find DCIS early.
The best chance of surviving breast cancer comes from the
early detection of carcinoma tumors through regular clinical breast exams and
mammograms. Reducing the risk of the disease ever occurring, however, should be
every woman�s goal.
The importance of Early
Life in Breast Cancer Risk
The National Cancer Institute and U.S. Department of
Health and Human Services recommend that women in their forties and older
have mammograms every one to two years. A complete early detection plan
also includes monthly breast self-exams and clinical breast examinations
by a trained medical professional.
|
Ideally the prevention of breast cancer would start in
youth and young adulthood, as this period has been found to be extremely
important in determining a woman�s risk of developing breast cancer later in
life. Breast tissue during this time (from youth up until a woman gives birth to
her first child) appears to be more susceptible to elements that can cause cells
to subsequently become cancerous. Exposure to radiation is a good example. The
risk for adult breast cancer is very high for a girl under ten exposed to high
dose of radiation , moderate for a teenager, and small for a young adult.
Risk Factors
associated with breast

Cancer
To many woman it would seem that just about everything
affects the risk of developing breast cancer. While this is not the case, the
scientific community has come a long way in identifying many factors that
increase the risk of the disease. These factors can range from history to
lifestyle to reproductive variables.
Although there are few factors that substantially increase
a woman�s risk of breast cancer, most individually elevate or lower risk by only
a small amount. Risk factors have been categorized as ones over which:
-
a woman has control (such as alcohol consumption and use
of postmenopausal hormones) and
-
a woman doesn't have control (such as breast cancer
in an immediate family member and age at menarche). By knowing how each of
these factors affects her risk, a woman can take appropriate steps to try to
protect herself from the disease.
Factors that cannot be controlled :
These are a number of factors beyond a woman�s control that
affect her risk of developing breast cancer. Understanding these may lead a
woman to be more vigilant about those factors under her control and, if
necessary, seek more frequent check ups or screening tests.
AGE
Age is a well � established risk factor for breast cancer.
In general, the older a woman is,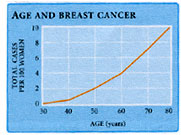 the greater her risk of the disease. the greater her risk of the disease.
In a group of I00 women who are fifty years old, 9 will
develop breast cancer before they reach the age of eighty. The I in 8 numbers
that many women recognize is the lifetime risk of breast cancer. This means that
for all adult women, I in 8 (or approximately I 2 percent) is at risk of
developing breast cancer in her lifetime. While a I2 percent lifetime risk is
high for a serious disease like breast cancer, the lifetime risk of coronary
heart disease is much higher (about 32 percent), and both coronary heart disease
and lung cancer kill more women overall.
FAMILY HISTORY AND GENETICS
It should come as no surprise that family is linked to the
risk of breast caner. Most people realize that the risk of many diseases are
associated with the experiences of their parents an siblings.
The age at which the mother was diagnosed, however,
influenced the level of risk as well .The younger the mother was when she was
diagnosed with the disease, the higher her daughter�s risk of developing breast
cancer. A woman whose mother was diagnosed before age forty has a large
increase in risk, while a woman whose mother was diagnosed after age seventy has
only a moderate increase in risk.
Family members usually have very similar lifestyles and
therefore may have similar �environmental �risk factors for breast cancer � such
as weight, activity level, and alcohol intake. While this may account for the
increased risk of breast cancer experienced by some families, in some cases
genetics likely plays a large role.
BENIGN BREAST DISEASE
The term benign breast disease is often used to describe a
wide range of non-cancerous conditions that can affect the breast. Two specific
types of benign breast disease � hyperplasia and radical scars � increase the
risk of developing breast cancer. Other benign breast conditions, such as cysts
and fibroadenomas, do not appear to influence risk.
BREAST DENSITY
The density of a woman�s breast has been shown in many
studies to be strongly related to the risk of breast cancer. Breast density is
most often assessed by mammogram and depends on the proportion of fat and tissue
that make up a woman�s breasts. When the X-rays used in a mammogram take an
image of the breast, fat appear dark and tissue appears light. Breasts with a
high density have a relatively high proportion of tissue and low proportion of
fat. Breasts with a low density have a relatively low proportion of tissues and
high proportion of fat.
Of note, one very large cohort study found that women with
the most dense breasts had approximately 5 times the risk of breast cancer
compared to women with the least dense breasts. And as breast density increased,
so did the risk of the disease.
RADIATION EXPOSURE IN CHILDHOOD OR ADOLESCENCE
Exposure to high doses of radiation to the chest in
childhood or adolescence has been consistently linked to an increased risk of
breast cancer in later adulthood. Studies have found that women who were exposed
in their youth to atomic bomb blasts (in Hiroshima or Nagasaki, Japan) or
radiation therapy for disorders like Hodgkin�s disease or tuberculosis had 2 to
4 times the risk of breast cancer compared to women who were not exposed to such
radiation. The greatest risk is generally in those women who were very young
when exposed, and the risk decreases as the age at the exposure increases. Women
over forty who have been exposed to high doses of radiation to the chest have
only a small increase in risk.
PERSONAL HISTORY OF CANCER
Just as family history can affect the risk of breast
cancer, so can a personal history of cancer. Women who have been previously
diagnosed with cancer in one breast are at increased risk of developing cancer
in the other breast.
Having a personal history of lobular carcinoma in situ �
which is usually not treated after diagnosis, just closely followed � also
increases the risk of cancer. Women with this condition are 7 to 10 times more
likely to develop breast cancer than women without the condition.
ETHNICITY
Not all groups of women in the United States are equally
impacted by breast lowest risk of Latina, Asian American Indian women tend to
have the lowest risk of breast cancer risk in the United States, and white women
tend to have the highest risk � followed closely by Hawaiian American and Africa
American can women.
For breast cancer occurring before midlife, however,
African American women are at highest risk. This is likely due, at least in
large part, to differences in the ages at which white women and African American
women first give birth.
HEIGHT
There is a substantial amount of evidence that height is
associated with the risk of breast cancer both pre- and postmenopause.
Height is generally thought to reflect, at least in part,
the quantity and quality of the diet in childhood . Well fed children generally
have more rapid, bigger growth spurts than children fed poor diets. This many
contribute to breast cancer risk because such rapid growth can increase the
chance that the DNA in some breast cells will become permanently damaged , which
can lead to cancer later in life .One other possibility is that levels of a
hormone called insulin � like growth factor are higher in taller children than
in shorter children . In some studies , high levels of insulin � like growth
factor have been linked to an increased risk of breast cancer.
Factors You Can Control:
It is important to know how all of the factors related to
breast cancer make up a woman�s risk. However, when given a choice, most women
would prefer to focus on those things they have control over and can change for
the better. These so-called modifiable factors are discussed in this section and
range from alcohol intake to use of postmenopausal hormones.
Vitamin A, Carotenoids, and Vegetables. A number of
studies have linked a low intake of
vitamin A and carotenoids, such as beta �
carotene, with an increased risk of breast cancer. Found in high amounts in
green and yellow vegetables and certain fruits, vitamin A is important for cell
growth, and carotenoids are powerful
antioxidants that can help protect cells
from the damaging effects of oxygen free radicals in the body.
Dietary Fat: Eating high amounts of total fat in
adulthood appears to have little, if any, effect on the risk of developing
breast cancer. According to a survey, It was found that women with a high
fat
diet do not have a greater risk of developing breast cancer .Similarly, women
who ate little fat (20 percent or less of total calories) did not have a lower
risk of the disease compared to women who ate a moderate amount. This analysis
found their neither a high fat diet nor a low fat diet was related to the risk
of breast cancer .
High intake of
monounsaturated fat (found in olive and
canola oil) has been found in some studies to lower the risk of breast cancer.
Estrogen Levels: Many modifiable factors can
increase the level of estrogen in the body, and therefore increase the risk of
breast cancer. Examples of such factors include gaining substantial weight as an
adult; being overweight and physically inactive after menopause ; drinking
modest amounts of alcohol ; or postmenopausal hormones .
Overweight and Weight Gain: Being overweight is
thought to increase the risk of breast cancer after menopause primarily by
increasing levels of the hormone estrogen. Although a woman�s ovaries stop
producing estrogen after menopause, her fat tissue converts estrogen precursors
to estrogen. The more weight put on after menopause, the more estrogen that is
produced . This relation of weight to hormone levels explains why breast cancer
risk in overweight postmenopausal women appears to be more pronounced in those
who have never taken postmenopausal hormones. The amount of estrogen contained
in postmenopausal hormones far outweighs that produced by the fat tissue in
overweight and obese women. Therefore, the full effect of weight on breast
cancer risk can become masked when a woman uses postmenopausal hormones. It is
not that taking postmenopausal hormones eliminates the risk of breast cancer
associated with being
overweight; it is that using hormones likely hides the
effect of weight on risk.
Body Shape: Body shape also seems to influence the
risk of breast cancer in postmenopausal women. Women who are apple � shaped �
those who tend to carry extra weight around the waist � seem to be at higher
risk of breast cancer than women who are pear � shaped � those who tend to carry
extra weight in their hips and thighs. Similar to the results of other studies,
we found that postmenopausal women with the largest waist sizes have about a 35
percent greater risk of breast cancer compared to those with the smallest waist
sizes. As with overall weight, the full effect of waist sizes on breast cancer
risk may be obscured by the use of postmenopausal hormones.
Physical Activity: Numerous studies have examined
the relationship between physical activity and breast cancer risk, but results
to data have been somewhat inconsistent. This variability in findings likely
relates to the different approaches researches use to assess a woman�s level of
physical activity, which can be difficult to measure accurately. Postmenopausal
women who engage in at least one hour of physical activity a day are I 5 to 20
percent less likely to develop breast cancer than women who are sedentary.
Physical activity may help lower the risk of breast cancer
in postmenopausal women by helping curb weight gain, which in turn helps keep
estrogen levels in check. In young girls, physical activity may have the added
benefit of putting off the age at which a girl first has period, therefore
reducing lifetime exposure to estrogen.
Alcohol: Drinking alcohol does not come without
accompanying risks especially for women. It has been found that even fewer than
2 drinks per day could increase risk. Compared to women who did not drink, those
who drank about half a drink to one drink a day had a small increase in the risk
of breast cancer , and those who drank more than one drink a day had a moderate
increase in risk .
Postmenopausal Hormones: A large number of U.S.
women take postmenopausal hormone therapy to alleviate the short � term symptoms
and longer � term health effects of menopause. While such hormones therapy
appears to be beneficial in many ways � lowering the risk of osteoporosis and
possibly coronary heart disease and colon cancer � it also increase the risk of
breast cancer in certain users.
Because postmenopausal hormones that contain only estrogen
have been shown to increase the risk of cancer of the uterus, more and women are
choosing to take hormones that contain both estrogen and progestin. It was
initially thought this combined therapy might reduce the excess risk of breast
cancer linked to postmenopausal hormones.
Birth Control Pills: The use of birth control pills
moderately increases the risk of breast cancer in those women who are currently
using them. Women who are currently taking the pill had a 50 percent increase in
risk compared to women who have never used the pill . Women who had used the
pill in the past (but were not doing so currently) did not show any increase in
breast cancer risk. Moreover, how long a woman had been on the pill did not seem
to change the results.
Although the pill seems to
slightly increase breast cancer risk in current users, it also has many
benefits. In addition to preventing unwanted pregnancy, it lowers the risk of
ovaries and endometrial cancers. Also, when women use the pill, it is during a
time in life when their absolute risk of breast cancer is low, so even though a
50 percent increase in risk is substantial, it will actually result in only a
few extra women developing breast cancer who otherwise would not have. Assessing
such individual risk and benefits and the impact they have on a woman�s
lifestyle is key to determining whether or not she sue birth control pills
Symptoms associated with Breast Cancer
The most common outward sign of breast cancer is a hard
lump in the breast that is usually not movable and may or may not be painful.
The skin over the lump may be thickened and dimpled (like the skin of an
oranges) or indented in areas where the cancer has spread. The nipple may be
inverted (turned inward) or leak dark fluid.
Possible symptoms of breast cancer include:
-
A lump or thickening in or near the breast or in the underarm area.
-
A change in the size or shape of the breast.
-
Thickening, swelling, distortion, or tenderness of the breast
-
Skin irritation or dimpling
-
Nipple pain, scaliness, ulceration, or retraction.
-
A change in the way the skin of the breast, areola, or nipple looks or
feels (for example, warm, swollen, red, or scaly).
-
Swelling or lump in armpit.
Breast pain is commonly due to benign conditions and is usually not the first
symptom of breast cancer.
Detecting Breast Cancer
Women should talk with their doctor about factors that can increase their
chance of getting breast cancer. Women of any age who are at higher risk for
developing this disease should ask their doctor when to start and how often to
be checked for breast cancer. Breast cancer screening has been shown to decrease
the risk of dying from breast cancer.
Women can take an active part in the early detection of breast cancer by:
-
Regular scheduled screening (Checking for
disease when there are no symptoms) by a doctor,
-
Mammograms
-
-
Clinical breast exams (breast exams performed by health professionals).
click here, for breast self-exams.
A screening mammogram is the best tool available for finding breast
cancer early, before symptoms appear. A mammogram is a special kind of x-ray.
Screening mammograms are used to look for breast changes in women who have no
signs of breast cancer. Mammograms can often detect a breast lump before it can
be felt. Also, a mammogram can show small deposits of calcium in the breast.
Although most calcium deposits are benign, a cluster of very tiny specks of
calcium (called microcalcifications - A tiny
deposit of calcium in the breast that cannot be felt but can be detected on a
mammogram. A cluster of these very small specks of calcium may indicate that
cancer is present) may be an early sign of cancer. before symptoms appear. A mammogram is a special kind of x-ray.
Screening mammograms are used to look for breast changes in women who have no
signs of breast cancer. Mammograms can often detect a breast lump before it can
be felt. Also, a mammogram can show small deposits of calcium in the breast.
Although most calcium deposits are benign, a cluster of very tiny specks of
calcium (called microcalcifications - A tiny
deposit of calcium in the breast that cannot be felt but can be detected on a
mammogram. A cluster of these very small specks of calcium may indicate that
cancer is present) may be an early sign of cancer.
Ultrasonography can often show whether
a lump is a fluid-filled cyst (not cancer) or a solid mass (which may or
may not be cancer). This exam may be used along with mammography.
If an area of the breast looks suspicious on the screening mammogram,
additional (diagnostic) mammograms may be needed. Depending on the results, the
doctor may advise the woman to have a
biopsy (The
removal of cells or tissues for examination under a microscope. When only a
sample of tissue is removed, the procedure is called an incisional biopsy or
core biopsy. When an entire lump or suspicious area is removed, the procedure is
called an excisional biopsy. When a sample of tissue or fluid is removed with a
needle, the procedure is called a needle biopsy or fine-needle aspiration).
Although mammograms are the best way to find breast abnormalities early, they
do have some limitations. A mammogram may miss some cancers that are present
(false negative) or may find things that turn out not to be cancer (false
positive). And detecting a tumor early does not guarantee that a woman's life
will be saved. Some fast-growing breast cancers may already have spread to other
parts of the body before being detected.
Most doctors recommend that women in their forties and
older should have mammograms regularly, every 1 to 2 years.
Colour doppler

Certain types of ultrasound machine show the blood supply to the lump and this
may help to distinguish between a cancer and a benign lump. The blood supply
shows up as patches of red or blue colour on the scan.
Blood tests
Samples of your blood will be taken to check your general health, the number of
cells in your blood (blood count) and to see how well your kidneys and liver are
working. Your blood may also be tested to see whether it contains particular
chemicals (called markers) which are sometimes produced by cancer cells
Some women perform monthly breast self-exams to check for any changes
in their breasts. When doing a breast self-exam, it's important to remember that
each woman's breasts are different, and that changes can occur because of aging,
the
menstrual cycle, pregnancy, menopause, or taking birth control pills or
other hormones. It is normal for the breasts to feel a little lumpy and uneven.
Also, it is common for a woman's breasts to be swollen and tender right before
or during her menstrual period. Women in their forties and older should be aware
that a monthly breast self-exam is not a substitute for regularly scheduled
screening mammograms and clinical breast exams by a health professional.
Grading of breast cancer
Grading refers to the appearance of the cancer cells under the microscope.
The grade gives an idea of how quickly the cancer may develop. There are three
grades:
-
grade 1 (low grade),
-
grade 2 (moderate grade) and
-
grade 3 (high grade).
Low grade means that the cancer cells look very like the normal cells of the
breast. They are usually slowly growing and are less likely to spread. In high
grade tumours the cells look very abnormal. They are likely to grow more quickly
and are more likely to spread.
Treatment Options for
Breast Cancer
Treatment of breast cancer varies according to the nature and extent of the
cancer, the opinion of the doctor or doctors and the wishes of the patient. To
play an active role in treatment decisions, a patient should gather as much
information as he or she can about a particular diagnosis. In some cases the
breast is removed completely along with surrounding tissues. This is called a
modified radical mastectomy, and for many years it was the only treatment
available. Now, in some cases in which the cancer is fairly small and localized
� which means it has not spread outside the breast � it is possible to remove
only the lump and some of the surrounding tissue. This procedure is sometimes
called a "lumpectomy." Lumpectomies are generally followed by radiation to the
breast. Sometimes chemotherapy may also be administered. For both mastectomy and
lumpectomy procedures, lymph nodes near the tumor are generally removed as well.
Patients with high risk breast cancer may be offered autologous blood stem
cell transplantation with a special treatment called the
Stamp V regimen.
Treatment(s) may involve:
-
Surgery - Any breast cancer surgery can be a deeply
traumatic experience. Surgery is used when a large number of cancer cells are together
in one place (usually the primary tumor) and when the surgeon can reach
that place without causing harm to the patient. Surgery is used to treat about
half of all cancers. To determine the degree to which the cancer may have
spread, the surgeon removes not only the obvious cancer, but a portion of what
appears to be healthy tissue around the cancer. Surgeons often remove the
lymph nodes that are near the cancer as well.
-
A
lumpectomy is a less invasive surgical
technique that involves removing the
tumor and the
lymph nodes (Hundreds of small bean
shaped organs (sometimes called glands) located throughout specific area of
the body in the lymphatic system. They act as filters to collect and destroy
bacteria. Cancer cells that may be moving through the lymphatic system can
get trapped in the lymph nodes) under the
arm but not the whole breast.
-
A
mastectomy can be segmental or
total. In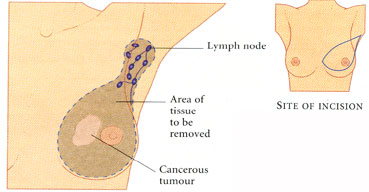 segmental mastectomy, the surgeon removes the cancer and a larger
area of normal breast tissue around it. Total mastectomy is more invasive and is
the surgical removal of the breast and the lymph nodes under the arm.
Breast reconstruction is often an option at the
same time as the mastectomy, or later on. Women considering reconstruction
should discuss this with a plastic surgeon before having a mastectomy. segmental mastectomy, the surgeon removes the cancer and a larger
area of normal breast tissue around it. Total mastectomy is more invasive and is
the surgical removal of the breast and the lymph nodes under the arm.
Breast reconstruction is often an option at the
same time as the mastectomy, or later on. Women considering reconstruction
should discuss this with a plastic surgeon before having a mastectomy.
-
Breast Conserving Surgery- an operation
conducted to remove the breast cancer but not the breast itself. Types of
breast-conserving surgery include
lumpectomy,
quadrantectomy, and
segmental mastectomy (removal of the cancer as well as some of the breast
tissue around the tumor and the lining over the chest muscles below the
tumor). Also called breast-sparing surgery.
-
Hormone therapy - Several types of cancer can only grow and spread in the
presence of natural chemicals in the body called hormones. Other types of
cancer, however, are slowed by specific hormones. The use of treatments that
fight cancer by altering the amounts of these hormones in the body is called
hormone therapy. This type of therapy is especially useful for treating
many cancers of the breast and reproductive system.
-
Chemotherapy- Chemotherapy is most often used when a cancer is not
isolated in one place but when it has metastasized
or spread throughout the body. Chemotherapy is also used to lessen the chances
that tumor cells that have spread, but can not be detected, will grow.
Chemotherapy is delivered to every tissue
in the body by the bloodstream. These drugs fight cancer by interfering with
the metabolism
or growth process of cancer cells, eventually causing the cells to die. For
many cancers, combinations of chemotherapy medicines are given because they
are more effective given together, than alone.
Chemotherapy regimens can be given in many ways, such as:
-
Oral (by mouth)
-
Topical (on top of the skin as a cream or lotion)
-
Intravenous (into a vein or IV)
-
Intraperitoneal (into the abdominal cavity or IP)
-
Intralesional (into the tumor)
-
Radiation therapy- Radiation is useful in treating many types of cancer.
It is often used when the cancer is in one, or a small number of places in the
body. Radiation therapy uses beams of high-energy waves or streams of
particles including
X-rays,
gamma rays, and
electrons to destroy cancer cells. Like chemotherapy, radiation therapy
halts the growth and division of cancer cells and causes them to die.
Two main types of radiation are used,
external beam radiation and internal radiation or
brachytherapy. External beam radiation focuses on the tumor from outside of the body. It
is much like getting a diagnostic X-ray, but for a longer time. Before
treatments start, imaging studies such as
MRIs,
CT
scans, or plain X-rays are done to find the exact location of the tumor.
The radiation team will then make some ink marks on the skin, that they will
later use as a guide, to focus the radiation in the right area. Each treatment
lasts only a few minutes and is painless.
Brachytherapy uses small radioactive pellets
or "seeds" that are placed near the tumor. Treatments are often combined with
external beam radiation, which is given at a lower dose than it normally would
be if used by itself.
5.
Biological therapy is a treatment designed to enhance the
body's natural defenses against cancer. For example, Herceptin� (trastuzumab) is
a monoclonal antibody (A
laboratory-produced substance that can locate and bind to cancer cells wherever
they are in the body. Many monoclonal antibodies are used in cancer detection or
therapy; each one recognizes a different protein on certain cancer cells.
Monoclonal antibodies can be used alone, or they can be used to deliver drugs,
toxins, or radioactive material directly to a tumor.) that targets
breast cancer cells that have too much of a protein known as human epidermal
growth factor receptor-2 (HER-2). By blocking HER-2, Herceptin slows or stops
the growth of these cells. Herceptin may be given by itself or along with
chemotherapy.
A woman's treatment options depend on a number of factors. These factors
include her age and menopausal status; her general health; the size and location
of the tumor and the stage (The extent of
a cancer within the body. If the cancer has spread, the stage describes how far
it has spread from the original site to other parts of the body.) of the
cancer; the results of lab tests; and the size of her breast. Often, two or more methods are used in combination.
In most cases a lumpectomy is followed by several weeks of :
-
Radiation, then chemotherapy, or
-
Hormone therapy, then radiation.
Things to Consider During
and After Treatment
During and after your treatment for breast cancer you may be able to speed up
your recovery and improve your quality of life by:
-
Taking an active role in the treatment process. Learn about the
benefits and risks of each of your treatment options, and ask questions of
your cancer care team if there is anything you do not understand. Learn about
and look out for side effects of treatment, and report these right away to
members of your cancer care team so they can take steps to ease them and
shorten their duration.
Remember that your body is as unique as your personality and your
fingerprints. Although understanding your cancer�s stage and learning about
your treatment options can help predict what health problems you may face, no
one can say for sure how you will respond to cancer or its treatment.
You may have special strengths such as a history of excellent nutrition and
physical activity, a strong family support system, or a deep faith, and these
strengths may make a difference in how you respond to cancer. There are also
experienced professionals in mental health services, social work services, and
pastoral services who may assist you in coping with your illness.
-
Opting for a healthy lifestyle: You can help in your own
recovery from cancer by making healthy lifestyle choices. If you use tobacco,
stop now. Quitting will improve your overall health and the full return of the
sense of smell may help you enjoy a healthy diet during recovery. If you use
alcohol, limit how much you drink. Have no more than 1 or 2 drinks per day.
Good nutrition can help you get better after treatment. Eat a nutritious and
balanced diet, with plenty of fruits, vegetables, and whole grain foods.
-
Rest: If you are being treated for cancer, be aware of the
battle that is going on in your body. Radiation therapy and chemotherapy
add to the fatigue caused by the disease itself. Give your body the rest it
needs so that you will feel better as time goes on. Exercise once you feel
rested enough. Ask your cancer care team whether your cancer or its treatments
might limit your exercise program or other activities.
-
It is important that you consider your emotional, psychological, and
spiritual health along with the physical aspects of your recovery from
cancer.
-
Side effects of treatment: A woman�s choice of treatment will
likely be influenced by her age, the image she has of herself and her body,
her hopes and fears, and her stage in life. For example, many women select
breast-conserving surgery with radiation therapy over a mastectomy for body
image reasons. On the other hand, some women who choose mastectomy may want
the affected area removed, regardless of the effect on their body image, and
others may be more concerned about the side effects of radiation therapy than
body image. Other issues that concern women include loss of hair from
chemotherapy and skin changes of the breast from radiation therapy. In
addition to these body changes, women may also be concerned about the outcome
of their treatment. These are all factors that affect how a woman will make
decisions about her treatment, how she views herself, and how she feels about
her treatment.
-
Concerns about sexuality are often very worrisome to a woman with
breast cancer. Some treatments for breast cancer can change a woman�s hormone
levels and may have a negative impact on sexual interest and/or response. A
diagnosis of breast cancer when a woman is in her 20s or 30s is especially
difficult because choosing a partner and childbearing are often very important
during this period. Relationship issues are also important because the
diagnosis can be very distressing for the partner, as well as the patient.
Partners are usually concerned about how to express their love physically and
emotionally during and after treatment.
A cancer diagnosis and its
treatment holds a major life challenge, with an impact on you and everyone who
cares for you.
Disease Management
If you are being treated for cancer, be aware of the battle that is going on
in your body. Radiation therapy and chemotherapy add to the fatigue caused by
the disease itself. Give your body the rest it needs so that you will feel
better as time goes on. Exercise once you feel rested enough. Ask your cancer
care team whether your cancer or its treatments might limit your exercise
program or other activities. It is important that you consider your emotional,
psychological, and spiritual health along with the physical aspects of your
recovery from cancer.
Women who have undergone treatment for breast cancer
should be reassured that their quality of life, once treatment has been
completed, will be normal.
|
Defining an Exercise Regime: Exercise for the
patient who has had breast surgery is important to the entire body and mind. But
specifically, it will speed up recovery from the effects of surgery. Any surgery
on the breast, whether a lumpectomy, removal of nodes under the arm, or a
mastectomy, will cause soreness and discomfort. While the immediate healing
process is occurring, exercise of the area (including the arm or shoulder)
should be at the physician's direction. Once healing is progressing, exercise
of the arm and shoulder is very important. The shoulder joint and the
muscles will tighten. If they are not used, their function will be limited. This
will lead to discomfort as well as unnecessary loss of use.
The Reach to Recovery Program of the American Cancer
Society has an excellent manual which gives specific exercises to assure a full
range of motion. These include reaching, pulling, and rotating the arm behind
the back to further stretch the shoulder joint. These exercises must be done on
a regular schedule to assure full use of the arm and shoulder. Programs using
aerobics and swimming can also accomplish the same results but should be done
under the direction of a knowledgeable instructor. You can also try innovative
forms of exercise: squeezing a ball with the hand, touching a board with the
feet, weight lifting with books. pulling, and rotating the arm behind
the back to further stretch the shoulder joint. These exercises must be done on
a regular schedule to assure full use of the arm and shoulder. Programs using
aerobics and swimming can also accomplish the same results but should be done
under the direction of a knowledgeable instructor. You can also try innovative
forms of exercise: squeezing a ball with the hand, touching a board with the
feet, weight lifting with books.
Becoming physically fit is an excellent way to enhance your
capacity to cope with the diagnosis and treatment of cancer. By striving for
your most realistic level of physical fitness, you become can get fit.
In the study, published in the American Journal of
Epidemiology(10 February, 2003), researchers from the German Cancer Research
Centre in Heidelberg said: "We found decreasing risks with increasing cycling
activity levels. They added: "For cycling, we found a significant protective
effect, and sports appeared to have some protective effect among otherwise less
active women." .It could be that cycling improves your immune system.
Nutritional Needs: The nutrient needs
of a cancer patient vary from person to person. Your doctor, nurses, and
dietitians can help you to identify your nutrition goals and plan strategies to
help you meet them. You need to eat a variety of foods that will provide the
nutrients you need to maintain your health while fighting cancer. These
nutrients include
protein,
carbohydrates,
fat,
water,
vitamins, and
minerals.
Eating a
balanced diet can be challenging when you are
receiving cancer treatment, particularly if treatment side effects persist for
long periods of time. Make use of the American Cancer Society Nutritional
Guidelines to plan what to eat each day.
-
Following surgery, chemotherapy, and radiation therapy,
additional protein is usually needed to heal tissues and to help prevent
infection. Eat high-protein foods first, when your appetite is strongest. Good
sources of protein include lean meat, fish, poultry, dairy products, nuts, dried beans, peas and lentils, and
soy foods.
meat, fish, poultry, dairy products, nuts, dried beans, peas and lentils, and
soy foods.
-
Eat five or more servings of a variety of vegetables and
fruits each day.
-
Choose whole grains in preference to processed (refined)
grains and sugars.
-
Limit consumption of red meats, especially those high in
fat and processed.
-
Choose foods that help you maintain a healthful weight.
-
Eat several small meals a day instead of three large meals.
-
Take interest in food by trying new recipes and products.
-
Drink beverages between meals instead of with meals.
-
Aim for eight glasses glasses of liquid each day.
In case of weight gain:
-
Select healthy foods including variety of vegetables,
fruits, whole grains, and beans.
-
Eat only when you're hungry. Eating to comfort feeling of
stress, fear or depression will not alleviate those emotions.
-
Pay attention to your portion-sizes.
Click here, for Suggestions For Healthy Eating After
Cancer
Spiritual Healing: Spirituality is
defined as caring for the "soul", and not every person believes in spirituality,
but to those who believe, faith and prayer have been shown to have a positive
affect. There is scientific research to suggest that it is possible to influence
health with the mind. In fact, mind/body interventions have become more popular
among mainstream medicine. Therapies like Tai Chi,
Meditation involve using the
mind and/or movements of the body as a source of healing. Meditation can
be done alone, or can be lead in a group. Meditation is excellent for
stress
reduction. Similar to meditation is guided visualization, which uses mental
imagery to let go of negative energy, and create positive images. Visualization
can be done alone, or can be lead by a professional or an audiotape.
For more and latest advances in Breast Cancer treatment,
click here
Emotional Health: The most common sexual side
effects stem from damage to a woman's feelings of attractiveness. In our
culture, we are taught to view breasts as a basic part of beauty and femininity.
If her breast has been removed, a woman may be insecure about whether her
partner will accept her and find her sexually pleasing. Therefore, it is
important that your focus on tests and treatments does not prevent you from
considering your emotional state.
-
A woman's choice of treatment will likely be influenced by her age, the
image she has of herself and her body, and her hopes and fears. For example,
some women may select breast-conserving surgery with radiation therapy over a
mastectomy for cosmetic and body image reasons. On the other hand, some women
who choose mastectomy may want the affected area removed, regardless of the
effect on their body image. They may be more concerned about the effects of
radiation therapy than body image. Your doctor will tell you when you have
healed enough to be fitted for a permanent breast form or prosthesis.
-
Other issues that women worry about include hair loss from
chemotherapy and skin changes of the breast from radiation therapy. In
addition to these body changes, women may also be dealing with concerns about
the outcome of their treatment.
-
It is important to remember that some treatments for breast cancer,
such as chemotherapy, can change a woman's hormone levels and may negatively
affect sexual interest and/or response. A diagnosis of breast cancer when a
woman is in her 20s or 30s is especially difficult because choosing a partner
and childbearing are often very important during this period.
-
Relationship issues are also important because the diagnosis can be very
distressing for the partner, as well as the patient. Partners are usually
concerned about how to express their love physically and emotionally after
treatment, especially surgery. Breast surgery will not affect your physical
ability to have sex, the accompanying strong emotions may affect your
sexual feelings for a while. Women often need to feel relatively happy with
their bodies to have a fulfilling sex life. Fear that a partner -- even a
long-standing one -- may be put off by the result of the surgery can make
women fearful of the moment they allow someone to see or touch their body.
There is no right or wrong time to take this step. When you do it, and the way
you do it, depend entirely upon your own feelings and your relationships.
Suggestions that may help a woman adjust to changes in her body image include
looking at and touching herself; seeking the support of others, preferably
before surgery; involving her partner as soon as possible after surgery; and
openly communicating feelings, needs, and wants created by her changed image.
This section has dealt mainly, and briefly, with the immediate emotional
impact of breast cancer surgery. This is not meant to imply that in a few months
you should feel fine and have fully accepted the changes to your body. The
emotional rollercoaster often lasts longer: you may find all your anxieties
returning each time you have to go for a follow-up appointment. New situations
may bring fears, anger and insecurities flooding back; women without a partner,
for example, may be particularly anxious if and when the time comes to get
sexually involved with someone.
Reducing Your Risk of
Breast Cancer
There are many things that can be done that may
help reduce your risk of breast cancer:
-
Reduce your dietary fats. High levels of
dietary fat have been linked with a higher incidence of breast and colon
cancer. Limit red meat to two or three servings per week and choose
low-fat dairy products. Fat intake should be no more than 30% of your
total daily food intake.
-
Increase fiber intake. A diet higher in
fiber is automatically lower in fat. Increase your fiber intake by:
1. Eating high-fiber cereal for breakfast every day
2. Snacking on fresh fruits and vegetables
3. Using whole grain breads and brown rice
4. Including legumes, beans and whole grains in your soups and salads
-
Eat a well-balanced diet. Be sure to
include foods that have vitamins A, C and E and Selenium, all of which
have been found to possibly offer some protection against cancer. Don�t
smoke, and drink alcohol only in moderation.
Decrease caffeine if bothered by lumpy, tender breasts with symptoms
becoming worse just before your period. Caffeine is found in coffee, tea,
colas, chocolate and some medicines.
-
Decrease weight, especially if you are
20 pounds or more overweight. Obese women are at an increased risk for
having both breast and uterine cancer.
-
Learn to cope with stress in your life
and reduce its harmful effects. Coping mechanisms include exercise,
relaxation, friendships and hobbies. Researchers now believe that
difficulty handling stress may lead to an increase in health problems,
including cancer.
-
Women at high risk should talk with
their doctor about other things that can be done to reduce their risk,
such as: getting their first mammogram before age 40, mastectomy and
taking Tamoxifen or Raloxifene.
Breast Cancer &
Pregnancy:
Pregnancy usually is safe for women
who are free of cancer and not undergoing treatment.
Several studies now have shown that getting pregnant after successful
treatment for breast cancer doesn't increase the risk of a cancer recurrence
or death, at least in women who had small tumors and negative lymph nodes.
For example, one study from the University of Washington paired up 53 women
who became pregnant after a breast cancer diagnosis with other women who had
similar breast cancer histories but who didn't become pregnant later. The
researchers found no evidence that getting pregnant had an adverse effect on
survival.
Many doctors still suggest that women wait two years after diagnosis with
breast cancer before trying to have a baby. The two-year period is used
because most recurrences happen during that time, which might affect a
woman's decision to become a mother.
|









