![]()
According to a year long study, while all types of obesity-related surgery are risky and a last option for most obesepeople, particularly older patients, vertical gastrectomy is preferred over three other methods (especially for those over 50).
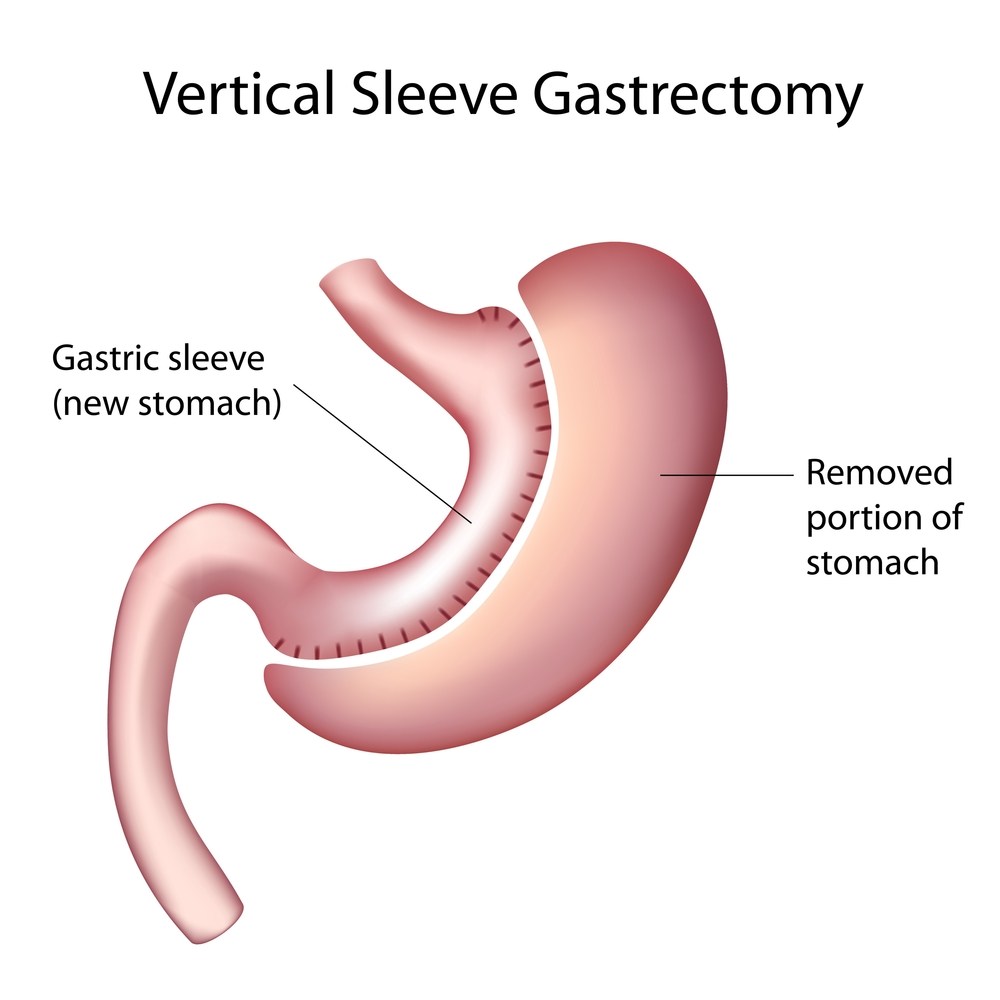
The stomach is the digestive organ that is connected between the esophagus and the small intestine. Food enters the stomach through the esophagus where it is broken down and then transferred to the small intestine where the nutrients are absorbed. Vertical gastrectomy (surgical removal of all or part of the stomach.) removes up to 95 percent of the stomach and leaves behind a thin tube-like stomach roughly 2 ounces (60 milliliters) in volume.
The other three types of surgery in order of the average amount of weight loss that resulted were Roux-en-Y gastric bypass, in which most of the stomach is sectioned off by a line of staples and part of the small intestine bypassed to inhibit the absorption of calories; duodenal switch, in which a large portion of the stomach is removed and the small intestine rearranged; and lap-band surgery, in which a silicone band is placed around the upper section of the stomach to shrink the stomach’s size and slow the exit of food.
The Vertical Gastrectomy is a reasonable solution to morbid obesity (BMI greater than 60Kg/M2). It can usually be done laparoscopically in patients weighing over 500 pounds. The stomach restriction that occurs allows these patients to lose more than 100 pounds and in many patients more than 200 pounds. This weight loss allows significant improvement in health and effectively “downstages” a patient to a lower-risk group. Once the patient’s BMI is lower (35-40) they can return to the operating room for the “second stage” of the procedure, which can either be the Duodenal Switch, Roux-en-Y gastric bypass or even a LapBand®.
Procedure
The Vertical Gastrectomy procedure is also called vertical Sleeve Gastrectomy, Greater Curvature Gastrectomy, Parietal Gastrectomy, Gastric Reduction, and even Vertical Gastroplasty. The excess stomach volume is removed, not left in place. This possibly eliminates most Ghrelin hormone production and helps to reduce the sensation of hunger that people have.
In this gastric restrictive procedure, the stomach is segmented along its vertical axis. To create a durable reinforced and rate-limiting stoma at the distal end of the pouch, a plug of the stomach is removed and a propylene collar is placed through this hole and then stapled to itself. Because the normal flow of food is preserved, metabolic complications are rare. Vertical banded gastroplasty may be performed using an open or laparoscopic approach.
The stomach that remains is shaped like a banana and measures from 2-5 ounces (60-150cc) depending on the surgeon performing the procedure. The nerves to the stomach and the outlet valve (pylorus) remain intact with the idea of preserving the functions of the stomach while reducing the volume. Note that there is no intestinal bypass with this procedure, only stomach reduction
Advantages of the Vertical Gastrectomy Weight Loss Surgery
- The stomach is reduced in volume but tends to function normally so most food items can be consumed, albeit in small amounts.
- Eliminates the portion of the stomach that produces the hormones that stimulate hunger (Ghrelin).
- No dumping syndrome because the pylorus is preserved.
- Minimizes the chance of an ulcer occurring.
- By avoiding the intestinal bypass, the chance of intestinal obstruction (blockage), anemia, osteoporosis, protein deficiency, and vitamin deficiency are almost eliminated.
- Very effective as a first-stage procedure for high BMI patients (BMI>55 kg/m2).
- Limited results appear promising as a single-stage procedure for low BMI patients (BMI 35-45 kg/m2).
- Appealing option for people with existing anemia, Crohn’s disease, and numerous other conditions that make them too high risk for intestinal bypass procedures.
- Can be done laparoscopically in patients weighing over 500 pounds.
Disadvantages of the Vertical Gastrectomy Weight Loss Surgery
- Potential for inadequate weight loss or weight regain. While this is true for all procedures, it is theoretically more possible with procedures that do not have an intestinal bypass.
- Higher BMI patients will most likely need to have a second-stage procedure later to help lose the rest of the weight. Two stages may ultimately be safer and more effective than one operation for high BMI patients. This is an active point of discussion for bariatric surgeons.
- Soft calories such as ice cream, milkshakes, etc can be absorbed and may slow weight loss.
- This procedure does involve stomach stapling and therefore leaks and other complications related to stapling may occur.
- Because the stomach is removed, it is not reversible. It can be converted to almost any other weight loss procedure.
- Considered investigational by some surgeons and insurance companies.
Complications
Complications include esophageal reflux, staple line disruption, and dilation or obstruction of the stoma, with the latter three requiring reoperation. Dilation of the stoma is a common reason for weight gain. While this procedure was once the most common kind of gastric restrictive procedure performed in this country, it has fallen out of favor due to a high reoperation rate.
Post-Op Dietary Plan for Vertical Gastrectomy Weight-Loss Surgery Patients
Patients must stick to a liquid-based diet for 2 weeks after surgery; 4-6 weeks after the operation, patients graduate to a 600-800 calorie/ day solid diet. Once the goal weight is achieved, usually 1-2 years after surgery, most patients can consume about 1000-1200 calories per day.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.



