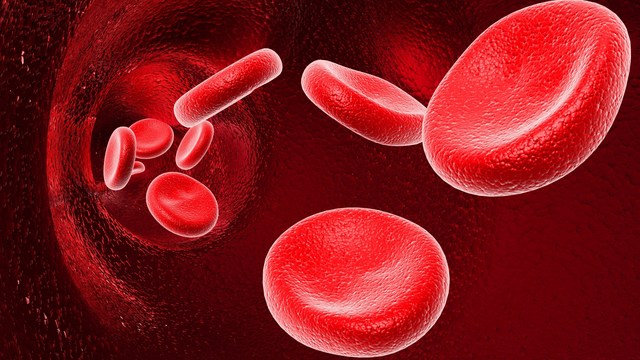
Rh factor is an inherited protein, found on the surface of red blood cells. If a person has the protein, they are Rh positive. Those who do not have the Rh protein are Rh negative. Rh factor positivity is very common. If a woman who is Rh negative and a father who is Rh positive conceive a child, the fetus may be Rh positive. This can lead to Rh incompatibility and pregnancy complications.
If the mother is Rh-negative, her immune system treats Rh-positive fetal cells as if they were a foreign substance. The mother’s body makes antibodies against the fetal blood cells. These antibodies may cross back through the placenta into the developing baby. They destroy the baby’s circulating red blood cells. When red blood cells are broken down, they make bilirubin. This causes an infant to become yellow (or having jaundice). The level of bilirubin in the infant’s bloodstream may range from mild to dangerously high.
Rh incompatibility causes the destruction of red blood cells without other effects.
After birth, the infant may have:
- Yellowing of the skin and whites of the eyes (jaundice)
- Low muscle tone (hypotonia) and lethargy
Detecting Rh factor
Before delivery, the mother may have an increased amount of amniotic fluid around her unborn baby (polyhydramnios).
There may be:
- A positive direct Coombs test result
- Higher-than-normal levels of bilirubin in the baby’s umbilical cord blood
- Signs of red blood cell destruction in the infant’s blood
Problems Caused by Incompatibility
Even if small amounts of the mother’s blood is mixed with the blood of the fetus, problems can arise.
The blood could mix as a result of:
- The placenta becoming detached from the wall of the uterus wall during delivery
- Bleeding during pregnancy
- Manual rotation of a breech baby
- Abortion
- Ectopic pregnancy
- Miscarriage
- A fall, blunt trauma, or invasive prenatal testing.
Prenatal tests, such as an amniocentesis or chorionic villus sampling, may place a mother with Rh-negative blood at risk for mixing her baby’s potentially Rh-positive blood with her own. If this happens, an immune response known as Rh sensitization may occur in the mother. This means that the mother will recognize future Rh-positive cells as foreign and her immune system will attack them.
Her body will produce antibodies to fight future exposure to Rh factor, including the blood of her fetus. This can result in the fetus’ red blood cells being destroyed.

Treatment
Rh incompatibility can be prevented with the use of RhoGAM. Therefore, prevention remains the best treatment. Treatment of an infant who is already affected depends on the severity of the condition.
Infants with mild Rh incompatibility may be treated with phototherapy using bilirubin lights. IV immune globulin may be also be used. For infants severely affected, an exchange transfusion of blood may be needed. This is to decrease the levels of bilirubin in the blood.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.



