Post-Traumatic Stress Disorder been around for thousands of years but rather confusingly under many different names. The first documented case of psychological distress was reported in 1900 BCE, by an Egyptian physician who described a hysterical reaction to trauma. Previous terms for what we now call PTSD have included ‘shell shock’ during WWI, ‘war neurosis’ during WWII; and ‘combat stress reaction’ during the Vietnam War. It was in the 1980s that the term Post Traumatic Stress Disorder (PTSD) was introduced – the term we most commonly use today.
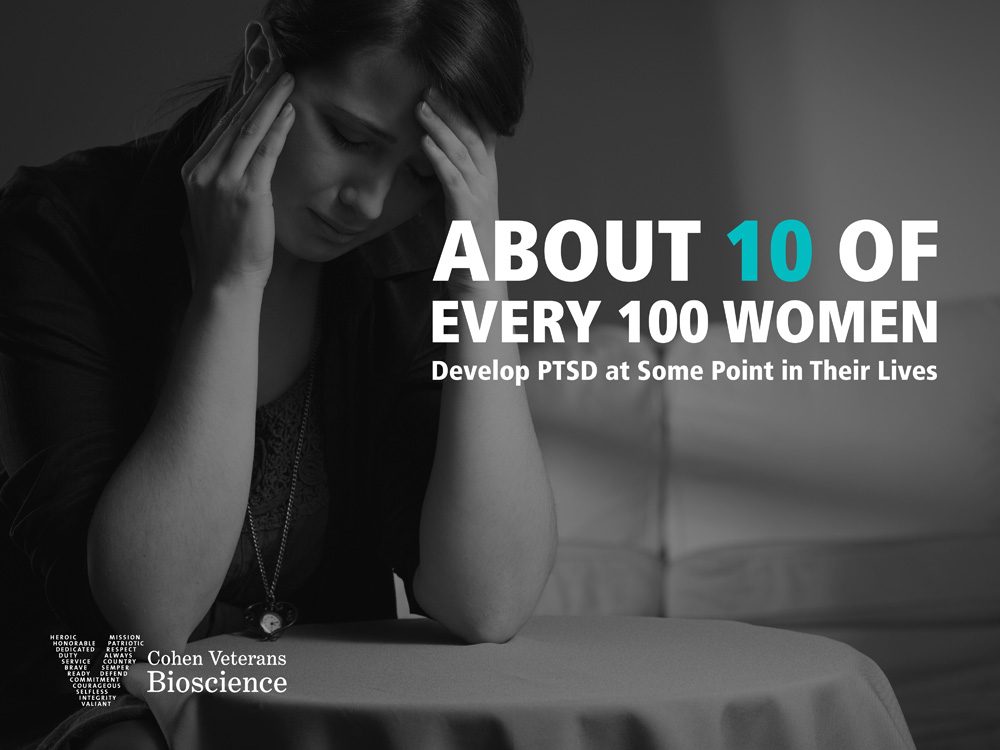
PTSD is essentially a memory filing error caused by a traumatic event. It’s worth pointing out that the majority of people exposed to a traumatic event experience short-term distress which resolves without the need for professional intervention. Unfortunately, the small proportion who do develop the disorder are unlikely to seek help and instead battle on despite their symptoms with their quality of life likely to be substantially reduced. Evidence suggests that there is around 70% of people in the UK do not receive any professional help and subsequently this debilitating disorder can also impacts upon loved ones, work colleagues and close friends.
The defining characteristic of a traumatic event is its capacity to provoke fear, helplessness, or horror in response to the threat of injury or death. Examples of traumatic events include:
- serious accidents •being told you have a life-threatening illness •bereavement •violent personal assault, such as a physical attack, sexual assault, burglary, robbery, or mugging •military combat •miscarriage •house fires •natural or man-made disasters •prolonged bullying •childhood neglect
Your exposure to traumatic event can happen in one or more of these ways:
- You experienced the traumatic event •You witnessed, in person, the traumatic event •You learned someone close to you experienced or was threatened by the traumatic event •You are repeatedly exposed to graphic details of traumatic events (for example, if you are a first responder to the scene of traumatic events).
At the time of the person being exposed to this intensely fearful situation, their mind ‘suspends’ normal operations as it copes as well as it can to survive. This might involve reactions such as ‘freezing to the spot’ or instead the opposite ‘flight away impetus’ from the danger. Until the danger passes the mind does not produce a memory for this traumatic event in the normal way because when the mind wishes to present the memory for filing it can be very distressing. The memories such as the facts of what happened, the emotions associated with the trauma and the sensations touch, taste, sound, vision, movement, and smell can be presented by the mind in the form of nightmares, flashbacks and intrusive unwanted memories. These re-experiences and flashbacks are a result of the mind trying to file the distressing memory, but understandably can be very unpleasant and frightening because they repeatedly expose the sufferer to the original trauma.
It’s like a filing cabinet at work. You’ve been too busy to complete all your filing one day, so you drop it in your bottom drawer. Each day, you’re still too busy to go back to that filing, but the bulging drawer reminds you need done, and it makes you anxious. When you finally try to do the filing, you realise there’re no reference numbers, you don’t who to ask for help, and you can’t read the documents to know where they should go, so you drop it back into your bottom drawer. This cycle will continue until you ask someone for help. Someone who can understand the documents and knows where they should be filed, or at the very least can help you find out what you need to know, in order to file them.”

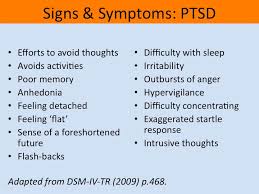
As the mind continues to try to process the memory, the individual also finds that his or her levels of awareness change. People can find it difficult to control their emotions and suffer intense symptoms of anxiety. This anxiety can present itself as both physical (shortness of breath, tight muscles, profuse sweating and a racing heart) as well as emotional (feeling on edge, hypervigilance (looking out for signs of danger all the time) or feeling panicky). There are many symptoms of PTSD.
Hyperarousal can increase emotional response, but many PTSD sufferers also feel emotionally numb and have trouble communicating with others about the way they feel – this may make them more anxious and irritable. Quite often, the feelings and symptoms of PTSD become so unmanageable and uncomfortable, that the sufferer starts to avoid anything linked to the original trauma which, as you can imagine, can affect day to day life.
The brain is programmed to process memories, and so the more the individual avoids things like thinking about the trauma, the less likely is it that any memory processing will occur, and the more likely it is that further attempts at filing a memory will occur automatically. This ultimately leads to further nightmares, flashbacks and intrusive memories which lead on to further hyper-arousal and emotional numbing, and this in turn leads on to more avoidance and so on. This is how the symptoms clusters perpetuate themselves in a vicious cycle which can go on for years – and why some PTSD sufferers ‘manage’ for such a long time without help, but eventually the symptoms become unmanageable.
Following a trauma, in the majority of people, the immediate psychological reactions settle down. In some people (thought to be 20% of those who suffer a trauma) these reactions can ‘stick’ and become chronic. If this is the case, PTSD may be said to be present. This theory is based in Horowitz’s Information Processing Model. ‘Research shows that PTSD isn’t just a psychological problem with a start, middle, and end, like many kinds of depression. Depression usually lasts around eight months but PTSD symptoms often worsen over time and are associated with adverse changes in the structure and function of the brain. For treatment to be successful, information processing must be completed. This is why therapies aimed at helping the individual to process and work through the traumatic material are extremely beneficial, however there are several types of treatment which can help those with PTSD.
Counselling – The Best Way Forward
It is widely believed that the best way forward is to start with counselling rather than use medication as the first and only solution to the problem. Recommended counselling approaches for PTSD include trauma-focussed cognitive behavioural therapy (CBT) and eye movement desensitisation and reprocessing (EMDR).
Both these approaches will help you to:
- learn ways to confront and come to terms with painful memories, thoughts and images, so you don’t feel as distressed by them
- learn strategies to help you get back into activities or visit places that you have avoided since the trauma because they have been too distressing
- learn tools to help you relax when you start getting too anxious or wound up
- explore thoughts that may be making your memories of the event more painful
Counselling can involve around 8 to 12 sessions, though in some cases it might take longer.
Medication for PTSD – what you need to know

The medications usually used to treat PTSD are antidepressants but even if you don’t have depression, antidepressants can help make feelings associated with trauma more manageable. There are different kinds of antidepressants, but research has shown that selective serotonin reuptake inhibitors (SSRIs) are most likely to help.
Before you start taking medication, you should be given information about possible side effects. It is also important to understand what you might experience if you stop taking medication suddenly, forget to take a tablet, or reduce the amount you are taking. Remember that antidepressants take a few weeks to reach their full effect, so do not expect immediate results.
If antidepressants are working, it is recommended that you take them for at least 12 months. After this period of time, you can stop by gradually reducing the dose. This should only be done after discussion with your GP, and should be carefully monitored. Remember, not all medication works in the same way for everybody. If a particular type of medication is not working for you, your doctor may ask you to try another type, increase the dose, or suggest that you try counselling.
What can I ask my GP about medication?
- How does this medication work? •What can I expect to feel like if it works? •Does it have any side effects and how long will they last for? •How long will it take before I start to feel better? •How long will I have to take it? •What do I do if I forget to take my medication? •When it’s time, how do I go about stopping the medication? •What will happen when I stop taking it? What if I don’t feel better when I expect to?
Some people with PTSD improve quickly, while others take more time to get better. PTSD can also feel manageable for a while, but worsen at times of stress or when a particularly strong reminder of the trauma triggers a reaction.
Sometimes things that happen during treatment can get in the way of your recovery, such as not receiving enough information about what to expect or not feeling comfortable with your GP or counsellor. It takes time to develop trust in someone, but if you continue to feel uncomfortable, discuss it with the person you are seeing or give yourself permission to look for the right person to provide you with help. Feeling overwhelmed by emotions during treatment can also get in the way of recovery. Let the person treating you know how you feel and talk with them about slowing down the process.
Stay safe and know that you are not alone in your thinking or emotions, PTSD is a common condition of the human heart and spirit and can be healed with help and support.
ALWAYS SEEK HELP IF YOU HAVE THE FOLLOWING SYMPTOMS
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.