The cervix is the neck of the womb (uterus). It connects the body of the uterus to the vagina (birth canal). The outside of the cervix and the vagina are covered by a layer of flat cells called squamous cells. The canal of the cervix is lined by tall column-like cells columnar cells. These two cell types, squamous cells and columnar cells, meet at a place called the squamo-columnar junction or the transformation zone. This junction may be on the outside of the cervix where it is easy to see. It is in this transformation zone that abnormal growth or dysplasia develops. The cervix plays an important role in maintaining a normal pregnancy. In non-pregnant women, the cervix has no obvious function.

When cervical cancer develops, the cells of the cervix become abnormal and grow out of control, and the cancercan spread to other parts of the body. But if abnormal cells are caught early, which they often are through the cervical screening programme, cancer can be prevented or treated.
- What is Cervical Cancer?
- Types of Cervical Cancer
- Causes of Cervical Cancer
- Symptoms of cervical cancer
- Diagnosis
- Treatment of Cervical Cancer
- Prevention
Cervical cancer is the sixth most common cancer in women.
Cervical cancers do not form suddenly. Normal cervical cells gradually develop precancerous changes that turn into cancer. This process usually takes many years but sometimes can happen in less than a year.
Most cervical cancers start at the transformation zone. Cervical intraepithelial neoplasia (CIN) is the term used to describe these abnormal changes. CIN is classified according to the degree of cell abnormality. Low-grade CIN indicates a minimal change in the cells and high-grade CIN indicates a greater degree of abnormality.
CIN may progress to squamous intraepithelial lesion (SIL; condition that precedes cervical cancer) or to carcinoma in situ (cancer that does not extend beyond the epithelial membrane). SIL is also classified as low-grade or high-grade. High-grade SIL and carcinoma in situ may progress to invasive carcinoma (cancer that has spread to healthy tissue).
There are 2 main types of cervical cancers: squamous cell carcinoma and adenocarcinoma.
About 80% to 90% of cervical cancers are squamous cell carcinomas, which are composed of cells that resemble the flat, thin cells called squamous cells that cover the surface of the endocervix. Squamous cell carcinomas most often begin where the ectocervix joins the endocervix.
10% to 20% of cervical cancers are adenocarcinomas. Adenocarcinomas are becoming more common in women born in the last 20 to 30 years. Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix. Less commonly, cervical cancers have features of both squamous cell carcinomas and adenocarcinomas. These are called adenosquamous carcinomas or mixed carcinomas.
Causes of Cervical Cancer:
The exact cause of cervical cancer is not known, but certain things appear to increase the risk.
- Human papilloma virus (HPV)
Specific types of the human papilloma virus are linked with 95% of cases of cervical cancer. This virus is passed from one person to another by skin-to-skin sexual contact. This means that body fluid is not needed to pass on the virus, but contact is enough to pass it on
- Sexual pattern & behaviour
Starting to have sex at an early age may expose the cervix to HPV at an especially susceptible time. Plus, the more sexual partners a woman has, the greater the risk of getting HPV. A history of sexually transmitted disease (STD) can be another primary cause. - The pill
The contraceptive pill may increase the risk of cervical cancer because barrier methods such as condoms, which give some protection from HPV, are less likely to be used. - Smoking
Women who smoke cigarettes are twice as likely to develop cervical cancer. Chemicals in cigarette smoke may increase the risk by damaging cervical cells.
- Unhealthy diet pattern
It is thought that diet can affect the risk. Also overweight women are more likely to develop this cancer. A healthy diet is recommended, including fruit, vegetables, fibre-rich and starchy foods.
- Immune deficiency
A weakened immune system increases the risk. Causes of immune deficiency include autoimmune diseases, such as rheumatoid arthritis, and human immunodeficiency virus (HIV) infection.
- History of abnormal cells
If abnormal cells (dyskaryosis) have previously been found on the cervix, women are at a higher risk.
- Multiple pregnancies:
Women who have had many full-term pregnancies have an increased risk of developing cervical cancer. - Family history of cervical cancer:
Recent studies suggest that women whose mother or sisters have had cervical cancer are more likely to develop the disease themselves. Some researchers suspect this familial tendency is caused by an inherited condition that makes some women less able to fight off HPV infection than others.
However, many women who have cervical cancer do not appear to have any of these risk factors.

Signs & Symptoms of cervical cancer:
There are no obvious signs or symptoms of cervical cancer. It tends to grow slowly over time.
Abnormal cells found on the end of the cervix during a cervical smear test are generally at an “early warning” pre-cancer stage, and do not cause any symptoms. These early abnormal cells are called cervical intraepithelial neoplasia (CIN). Treating CIN prevents cancer developing.
If abnormal cells do develop into cervical cancer, it can cause these symptoms:
- Abnormal vaginal bleeding, such as between periods or after intercourse bleeding between menstrual periods, increased menstrual bleeding
- Vaginal bleeding after the menopause
- Smelly vaginal discharge – pale, pink, brown, blood streaked, and foul-smelling
- Discomfort and pain during intercourse (dyspareunia)
- Painful urination (dysuria)
It is important for women experiencing any of these symptoms to see a doctor, even though their cause is usually not cervical cancer.
Cervical cancer that has spread (metastasized) to other organs may cause constipation, blood in the urine (hematuria), abnormal opening in the cervix (fistula), and ureteral obstruction (blockage in the tube that carries urine from the kidney to the bladder).
Diagnosis of cervical cancer includes a Papanicolaou test (Pap smear) and pelvic examination. The American Cancer Society recommends that all women begin having annual Pap smears at the age of 18, or when they become sexually active. After three consecutive negative tests, health care practitioners may perform the test less often (e.g., every 2 or 3 years). The American College of Obstetrics and Gynecology recommends a yearly Pap smear for all women who are sexually active.
In a Pap smear, the health care practitioner removes cells from the surface of the cervix using a spatula, cotton swab, or brush. The cells are placed on a glass slide for microscopic evaluation in a laboratory. For accurate results, the test should be performed 2 weeks after the end of a menstrual period and at least 48 hours after sexual intercourse.
Some health care practitioners confirm the presence of cervical lesions with colposcopy. After the Pap smear is performed, the cervix is washed with a diluted vinegar solution and examined for abnormalities using a light and a magnifying device (a colposcope). If abnormal areas are detected, further evaluation is necessary, regardless of the results of the Pap smear. Colposcopy takes a few minutes to perform and may not be covered by insurance.
In a pelvic examination, the vagina and adjacent organs are examined visually and bimanually (using both hands). Visual examination is performed using a speculum (instrument that is warmed and used to separate tissue) inserted into the vagina. Next, the organs are palpated (felt with the fingers) by inserting gloved fingers of one hand into the vagina and placing the other hand on the abdomen.
Other Diagnostic Tests
If low-grade CIN is detected, the Pap smear is repeated in 3-6 months and the patient is tested for HPV infection. If high-grade CIN is detected, colposcopy and biopsy may be performed. In colposcopy, abnormal lesions on the cervix are examined using a magnifying device. In biopsy, cells are removed for microscopic examination.
If invasive cervical cancer is suspected, or if the colpscopy and Pap smear results differ, cone biopsy or endocervical curettage may be performed. In cone biopsy, a larger, cone-shaped sample of cervical tissue is removed and examined for cancer cells. In endocervical curettage, the lining of the cervical canal is scraped and examined for cancer cells.
Once a diagnosis of cervical cancer is made, the cancer is staged. Staging involves a pelvic examination, blood tests, and imaging procedures. Blood tests may include a complete blood count (CBC) and serum chemistry to evaluate kidney and liver function.
Imaging procedures may include the following:
- Chest x-ray
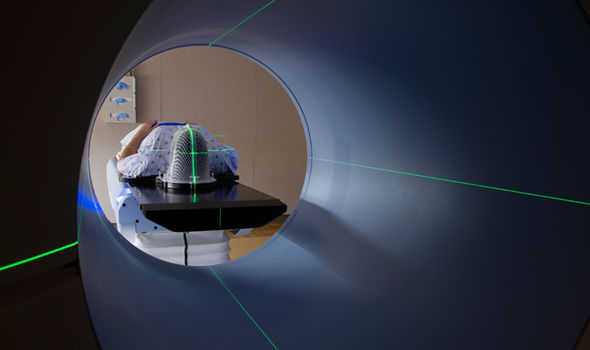
- CT scan of the pelvis and abdomen
- Cystoscopy and proctoscopy
Stage 1: Cancer cells are only found in the cervix.
Stage 2: The cancer has begun to spread beyond the cervix into surrounding tissues.
Stage 3: The cancer has spread deeper into other tissues of the pelvis, for example into the lower part of the vagina or nearby lymph nodes. It may press against a ureter (the tubes that drain kidneys), blocking it and preventing the kidney from draining.
Stage 4: The cervical cancer cells have spread to other organs such as the bladder, bowel or, more rarely, beyond the immediate area of the pelvis to the lungs, liver or bones.
Treatment options for cervical cancer include surgery, radiotherapy and chemotherapy. There are many factors that determine the type of treatment recommended. These include a woman’s age and general health, as well as the exact type and stage of cancer.
In early stages of the disease either surgery (hysterectomy) or radiotherapy, or a combination of both might be appropriate. For more advanced disease, radiotherapy is necessary, and may be used in combination with chemotherapy
In cases of cervical intraepithelial neoplasia (CIN), abnormal tissue may be removed using loop electrode excision (using wire loops heated by electric current) or cone biopsy. Carcinoma in situ may be removed using loop electrode excision, cryosurgery, or laser ablation. In cryosurgery, liquid nitrogen is circulated through a probe, which is applied to cancerous tissue. Freezing temperatures destroy the cancer cells. Laser ablation involves using a laser (device that emits intense heat and light at close range) to remove cancerous tissue.
Surgical treatment for invasive cervical cancer is radical hysterectomy, which is the removal of the uterus, fallopian tubes, ovaries, adjacent lymph nodes, and part of the vagina. If cancer has spread (metastasized) to lymph nodes in the abdomen, lymphadenectomy (surgical removal of lymph nodes) may also be performed. It is a major surgical procedure and is performed under general anaesthesia. A hospital stay of 5 to 7 days is common for an abdominal hysterectomy, and complete recovery takes about 4 to 6 weeks. Complications are unusual but could include excessive bleeding, wound infection, or damage to the urinary and intestinal systems. A radical hysterectomy and pelvic lymph node dissection are the usual treatment for stages IA2, IB, and IIA cervical cancer, especially in young people.
Radiation therapy uses high energy x-rays to kill cancer cells. These x-rays may be given externally in a procedure that is much like having a diagnostic x-ray. This is called external beam radiation therapy. This treatment usually takes 6 to 7 weeks to complete.
The skin in the treated area may look and feel sunburned, but this gradually fades to a tanned look, returning to a normal appearance in 6 to 12 months.
The second type of radiation therapy is called brachytherapy. It may be given as a capsule of radioactive material placed in the vagina near the tumor, or the radioactive material may be placed in thin needles that are inserted directly in the tumor. Both of these are done with the patient under anesthesia. Brachytherapy is completed in just a few days.
Many women also notice tiredness, upset stomach, or loose bowels. Pelvic radiation therapy may cause vaginal stenosis (narrowing of the vagina by scar tissue), which might make intercourse painful. Premature menopause and problems with urination may also occur.
If you are having side effects from radiation, discuss them with your cancer care team. There are things you can do to get relief from these symptoms or to keep them from happening, such as using vaginal dilators to manage vaginal stenosis.
Chemotherapy
Systemic chemotherapy uses anticancer drugs that are injected into a vein or given by mouth. These drugs enter the bloodstream and reach all areas of the body, making this treatment potentially useful for cancers that have spread to distant organs.
Drugs most often used in treating cervical cancer include cisplatin, paclitaxel, ifosfamide, hydroxyurea, fluorouracil, and irinotecan. If chemotherapy is chosen, you may receive a combination of drugs. Chemotherapy drugs kill cancer cells but also damage some normal cells, which can lead to side effects.
Chemotherapy side effects depend on the type of drugs, the amount taken, and the length of time you are treated. Temporary side effects of chemotherapy might include:
- Nausea and vomiting
- Loss of appetite
- Loss of hair
- Mouth sores
Most side effects of chemotherapy (except premature menopause and infertility) disappear once treatment is stopped. Hair will grow back after treatment ends. Premature menopause can be treated with hormones.
Choosing a healthy lifestyle and environment can help you prevent cancer.
Avoiding sexual activity that increases the risk for HPV infection, not smoking, and having regular Pap smears can help prevent most cases of cervical cancer. Using barrier contraception (e.g., condoms) and limiting the number of sexual partners may prevent HPV infection.
Read about Cervical cancer vaccines (also called Human Papillomavirus or HPV vaccines) protect against the virus that causes almost all cervical cancers.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.



