Pain is the first sign that something is wrong with the body. Did you know that the source lies in your brain?
Anxiety, stress, and depression are problems for an estimated 30 to 45 percent of patients with chronic back pain, and an even higher percentage of back-pain patients who experienced early childhood adversity.
In a revelation that set the international media abuzz, Apkarian’s group found that the anatomy of the human brain in patients who suffered from chronic pain was abnormal. In those who had suffered for five years, both the hippocampus and the prefrontal cortex were structurally transformed, sacrificing 5 to 11 percent of their grey matter density.
How does Your Brain Respond to Pain?
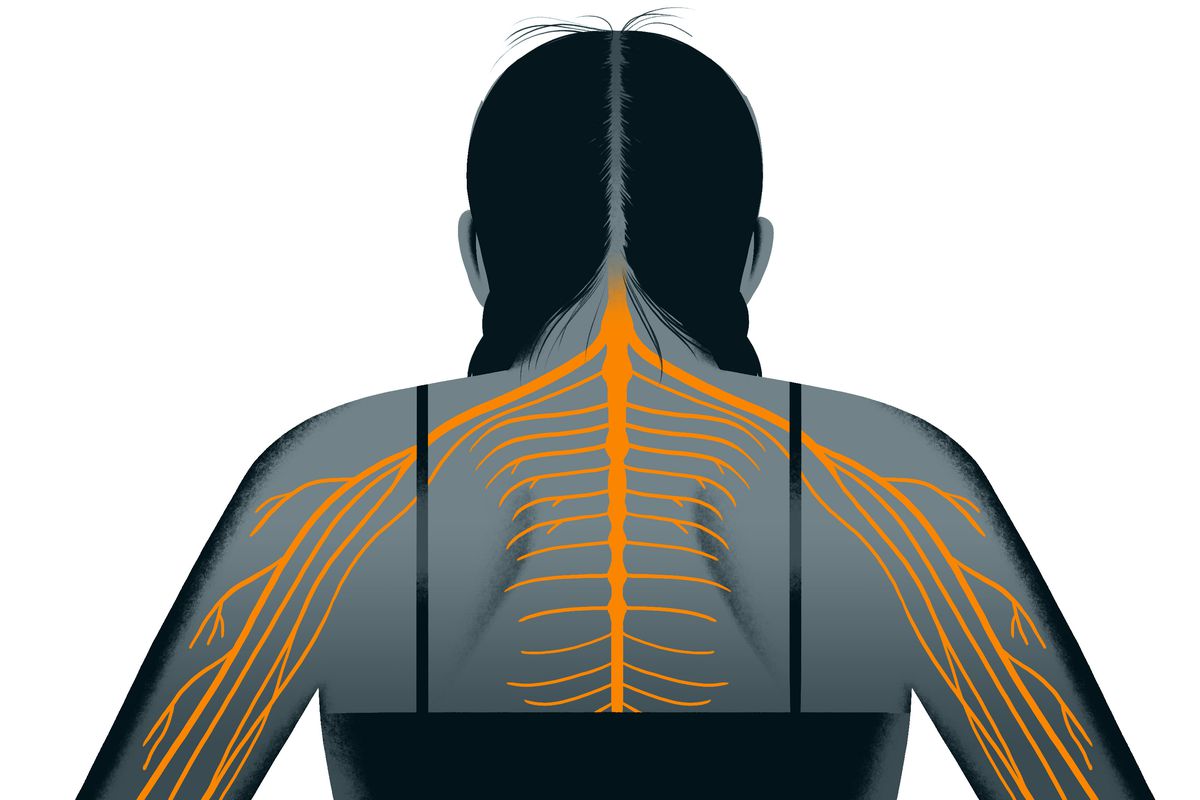
Once a pain signal reaches the brain, a number of things can happen. Certain parts of the brain stem (which connects the brain to the spinal cord) can inhibit or muffle incoming pain signals by the production of endorphins, which are morphine-like substances that occur naturally in the human body. Stress, excitement, and vigorous exercise are among the factors that may stimulate the production of endorphins. The impact of endorphins is why athletes may not notice the pain of a fairly serious injury until the “big” game is over. It is also why regular low-impact aerobic exercise (e.g. a riding stationary bike) can be an excellent method to help control chronic back pain.
Types of Pain
Every kind of pain falls into four basic categories.
- There’s nociceptive pain, the normally short-lived kind you feel when you accidentally slam your finger in the car door.
- There’s inflammatory pain, a response to damage or infection, resulting in a rush of small proteins called inflammatory cytokines to the site of the casualty. That pain has a habit of spreading, to affecting everything in the vicinity.
- Beyond that, there’s neuropathic pain, known as ‘radiculopathy’. It results, usually, from an insult to a nerve, culminating in burning, tingling, or shock-like sensations that travel the length of the affected nerve (sciatic pain is a good example).
- When any of those three types of pain sticks around long after the inciting injury has healed – or in the absence of any noxious stimulus – the patient can be said to be suffering from ‘central sensitisation’. Central sensitisation is a condition in which even mild injury can lead to a hyperactive and persistent response from the central nervous system.
According to the neuroscientist A Vania Apkarian, a professor of physiology, anesthesiology, and physical medicine at Northwestern University’s Feinberg School of Medicine in Chicago, “The brain of a person with lower-back pain looks different from that of a person with a repetitive-stress injury.”
Subsequently, more than 50 studies, most from other investigators, have documented regional decreases in grey matter density, volume, or thickness. Beyond that, the neuronal network of the remaining grey matter is rearranged, in patterns that are specific to chronic-pain conditions.
Treating Pain
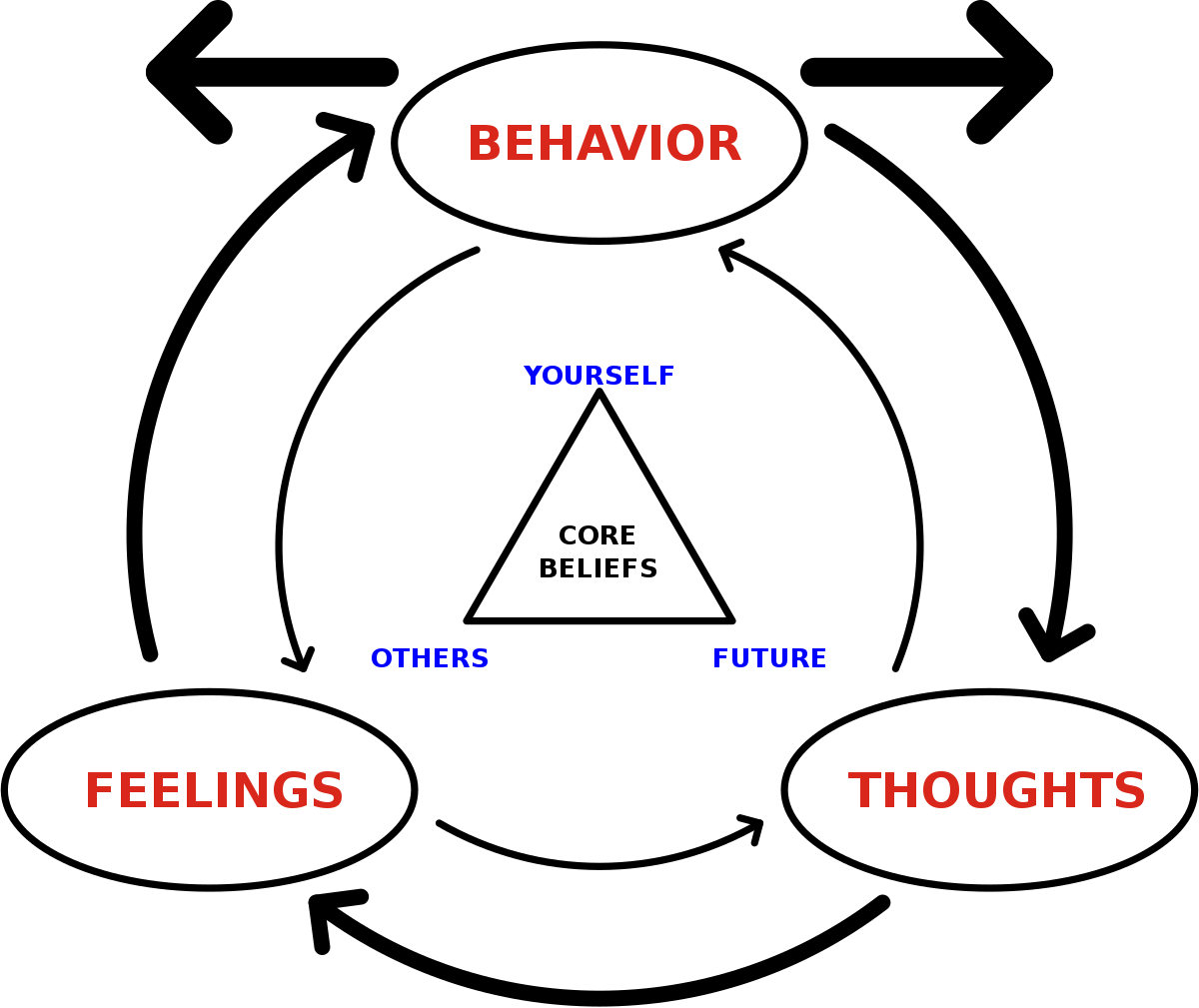
Many pain psychologists and rehab specialists believe that central sensitisation can be successfully treated with a combination of
- Cognitive Behavioural Therapy (CBT) and
- Graded non-pain-contingent exercise.
More about CBT:
CBT treatment usually involves efforts to change thinking patterns. These strategies might include:
- Learning to recognize one’s distortions in thinking that are creating problems, and then reevaluate them in light of reality.
- Gaining a better understanding of the behavior and motivation of others.
- Making use of problem-solving skills to cope with difficult situations.
- Learn to develop a greater sense of confidence in one’s own abilities.
The treatment also usually involves efforts to change behavioral patterns. These strategies might include:
- Facing one’s fears instead of avoiding them.
- Using role-playing to prepare for potentially problematic interactions with others.
- Learning to calm one’s mind and relax one’s body.
Depending on the kind of chronic-pain rehab programme you enter, you might find yourself hauling around a plastic milk crate filled with steel bricks, engaging in water aerobics, doing reps with free weights, or pushing an industrial sled (a heavy aluminum rectangle equipped with sliders on its base and sturdy handles on either end) or playing a game of beach volleyball, all under the close but generally unsympathetic supervision of someone who understands how bodies work and has seen it all before. The grimacing, the groaning, the odd body mechanics – all of them must go.
Strengthening must follow. And when it does, you will be rewarded with a sense of mastery over your own body, and no longer feels like a helpless victim.
Ref:
- https://www.spine-health.com/conditions/spine-anatomy/pain-signals-brain-spine
- https://aeon.co/essays/to-treat-back-pain-look-to-the-brain-not-the-spine
- https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
- https://www.vox.com/science-and-health/2017/10/2/16338094/dr-john-sarno-healing-back-pain
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.