|
|
Trigeminal Neuralgia : the compression of the nerve
Severe pain on one side of the face due to compression, inflammation, or
damage to the trigeminal nerve.
The trigeminal nerve transmits sensation from parts of the face
to the brain and controls some of the muscles that are involved in
chewing.
|
 TN
(Trigeminal Neuralgia / tic douloureux) is a disorder of the fifth cranial
(trigeminal) nerve that causes episodes of intense, stabbing, electric
shock-like pain in the areas of the face where the branches of the nerve are
distributed - lips, eyes, nose, scalp, forehead, upper jaw, and lower jaw. By
many, it's called the "suicide disease". TN
(Trigeminal Neuralgia / tic douloureux) is a disorder of the fifth cranial
(trigeminal) nerve that causes episodes of intense, stabbing, electric
shock-like pain in the areas of the face where the branches of the nerve are
distributed - lips, eyes, nose, scalp, forehead, upper jaw, and lower jaw. By
many, it's called the "suicide disease".
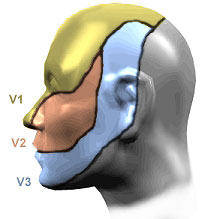
Where lies the Trigeminal Nerve
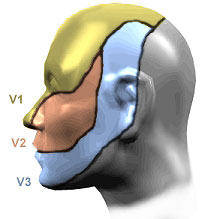 The
trigeminal nerve is the fifth of twelve pairs of cranial nerves enervating the
face and head, and is denoted by the Roman Numeral V. It has three divisions
which enervate the forehead and eye (ophthalmic V1), cheek (maxillary V2) and
lower face and jaw (mandibular V3). The trigeminal nerves function in sensing
facial touch, pain and temperature, as well as controlling muscles used for
chewing. The trigeminal nerve functions should be distinguished from the facial
nerve (cranial nerve VII), which controls all other facial movements. The
trigeminal nerve is the fifth of twelve pairs of cranial nerves enervating the
face and head, and is denoted by the Roman Numeral V. It has three divisions
which enervate the forehead and eye (ophthalmic V1), cheek (maxillary V2) and
lower face and jaw (mandibular V3). The trigeminal nerves function in sensing
facial touch, pain and temperature, as well as controlling muscles used for
chewing. The trigeminal nerve functions should be distinguished from the facial
nerve (cranial nerve VII), which controls all other facial movements.
The three divisions of the trigeminal nerve come together in an area called the
Gasserion ganglion. From there, the trigeminal nerve root continues back towards
the side of the brain stem, and inserts into the pons. Within the brain stem,
the signals traveling through the trigeminal nerve reach specialized clusters of
neurons called the trigeminal nerve nucleus. Information brought to the brain
stem by the trigeminal nerve is then processed before being sent up to the brain
and cerebral cortex, where a conscious perception of facial sensation is
generated.
There are seven forms of TN:
These forms of TN can be distinguished from idiopathic (atypical) facial pain,
as well as other disorders causing cranio-facial pain.
-
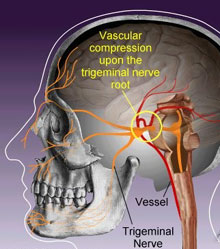 Typical
TN- This is the most common form of TN, that has previously been termed
Classical, Idiopathic and Essential TN. Nearly all cases of typical TN are
caused by blood vessels compressing the trigeminal nerve root as it enters
the brain stem. Typical
TN- This is the most common form of TN, that has previously been termed
Classical, Idiopathic and Essential TN. Nearly all cases of typical TN are
caused by blood vessels compressing the trigeminal nerve root as it enters
the brain stem.
-
Atypical TN-Atypical TN is characterized by a unilateral,
prominent constant and severe aching, boring or burning pain superimposed
upon otherwise typical TN symptoms. Some believe atypical TN is due to
vascular compression upon a specific part of the trigeminal nerve (the
portio minor), while others theorize that atypical TN represents a more
severe form or progression of typical TN.
-
Pre-TN- Days to years before the first attack of TN pain, some
sufferers experience odd sensations in the trigeminal distributions destined
to become affected by TN. These odd sensations of pain, (such as a
toothache) or discomfort (like "pins and needles", parasthesia), may be
symptoms of pre-trigeminal neuralgia. Pre-TN is most effectively treated
with medical therapy used for typical TN. When the first attack of true TN
occurs, it is very distinct from pre-TN symptoms.
-
Multiple-sclerosis-related TN- Two to four percent of patients
with TN have evidence of multiple sclerosis and about 1% of patients
suffering from multiple sclerosis develop TN. Those with MS-related TN tend
to be younger when they experience their first attack of pain, and the pain
progresses over a shorter amount of time than in those with typical TN.
Furthermore, bilateral TN is more commonly seen in people with multiple
sclerosis.
-
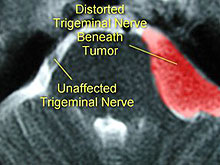
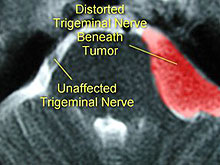
Secondary TN or Tumor Related Trigeminal Neuralgia- Trigeminal
neuralgia pain caused by a lesion, such as a tumor, is referred to as
secondary trigeminal neuralgia. A tumor that severely compresses or distorts
the trigeminal nerve may cause facial numbness, weakness of chewing muscles,
and/or constant aching pain (also see Trigeminal Neuropathy or
Post-Traumatic Trigeminal Neuralgia).
-
Trigeminal Neuropathy or Post-traumatic TN (trigeminal neuropathy)-
Trigeminal Neuropathy or Post-Traumatic TN may develop following cranio-facial
trauma (such as from a car accident), dental trauma, sinus trauma (such as
following Caldwell Luc procedures) but most commonly following destructive
procedures (rhizotomies) used for treatment of TN. Following TN injury,
numbness may become associated with bothersome sensations or pain, sometimes
called phantom pain or deafferentation pain. These pain conditions are
caused by irreparable damage to the trigeminal nerve and secondary
hyperactivity of the trigeminal nerve nucleus
-
Failed TN- Unfortunately, in a very small proportion of
sufferers, all medications, microvascular decompression and destructive
rhizotomy procedures prove ineffective in controlling TN pain. This
condition is called "failed" trigeminal neuralgia. Such individuals also
often suffer from additional trigeminal neuropathy or post-traumatic TN as a
result of the destructive interventions they underwent.
The pain of trigeminal neuralgia is due to a disturbance in the function
of the trigeminal nerve, which carries sensation from the face to the brain.
The cause of the pain is often unknown. But, the pain may occur when a blood
vessel comes in contact with the trigeminal nerve. This places pressure on the
main part of the nerve as it enters the brain.
Besides pressure by a blood vessel, other less frequent sources of pain to
the trigeminal nerve may include:
-
Compression by a tumor.
-
Inflammation, swelling and injury of the covering (myelin sheath) of the
trigeminal nerve in a process called demyelination. This occurs in people
with multiple sclerosis who develop trigeminal neuralgia.
Damage to this nerve causes repeated bursts of sharp, stabbing pain, known
as trigeminal neuralgia, in the lip, gum, or cheek on one side of the face.
Attacks may last for a few seconds or several minutes and may become more
frequent over time. An attack may occur spontaneously or be triggered by certain
facial movements, such as chewing, or by touching a trigger spot on the face.
Attacks rarely occur at night.
People who have experienced severe trigeminal neuralgia have described the
pain as:
-
Lightning-like
-
Shooting
-
Jabbing
-
Like having live wires in your face
It's possible for the pain to occur on both sides of your face, but
trigeminal neuralgia usually affects just one side. The pain may affect just a
portion of one side of your face, or the pain may spread in a wider pattern.
The condition also tends to come and go. You may experience attacks of pain
off and on all day, or even for days or weeks at a time. Then, you may
experience no pain for a prolonged period of time.
A variety of triggers, many subtle, may set off the pain.
These triggers may include:
-
Shaving

-
Stroking your face
-
Eating
-
Drinking a hot or cold liquid
-
Brushing your teeth
-
Talking
-
Putting on makeup
-
Encountering a slight breeze
-
Walking into an air-conditioned room
|
 No
one test can diagnose trigeminal neuralgia. The condition must be distinguished
from other forms of facial pain that may be due to diseases of the teeth, jaw or
sinuses. Magnetic resonance imaging (MRI) or computerized tomography (CT)
scans of the brain can eliminate some causes, such as tumors, aneurysms or
multiple sclerosis, all of which can cause trigeminal neuralgia in a small
number of people. No
one test can diagnose trigeminal neuralgia. The condition must be distinguished
from other forms of facial pain that may be due to diseases of the teeth, jaw or
sinuses. Magnetic resonance imaging (MRI) or computerized tomography (CT)
scans of the brain can eliminate some causes, such as tumors, aneurysms or
multiple sclerosis, all of which can cause trigeminal neuralgia in a small
number of people.
Your doctor will examine you to rule out any other causes of facial pain,
such as toothache or sinusitis .
A physician will ask for a description of the pain -- how severe it is, what
part of the face it affects, what seems to trigger episodes of pain. A
neurologic examination involves touching various parts of the face to determine
exactly where the pain is occurring and -- if it appears to be trigeminal
neuralgia -- which branches of the trigeminal nerve may be affected.
Medications are the typical initial treatment for trigeminal neuralgia.
Medications are often effective in lessening or blocking the pain signals sent
to your brain. A number of drugs are available. If you stop responding to a
particular medication or experience too many side effects, there's always the
potential to switch to another one.
 Your
doctor may prescribe painkillers, such as paracetamol or ibuprofen. Your
doctor may prescribe painkillers, such as paracetamol or ibuprofen.
However, if the pain persists, your doctor may prescribe anticonvulsant
drugs, such as carbamazapine, Phenytoin (Dilantin, Phenytex, Oxcarbazepine (Trileptal)
or certain antidepressants, all of which
have been shown to be effective in treating trigeminal neuralgia. Unlike
painkillers, which are taken only when the pain is present, both anticonvulsants
and antidepressants need to be taken every day to prevent attacks.
 Baclofen
(Lioresal) a muscle relaxant may be used in combination with carbamazepine or
phenytoin. Side effects include confusion, mental depression and severe
drowsiness. Baclofen
(Lioresal) a muscle relaxant may be used in combination with carbamazepine or
phenytoin. Side effects include confusion, mental depression and severe
drowsiness.
If a tumour is found, surgery may be necessary to remove it. Surgery may
also be used to separate the trigeminal nerve from a blood vessel if the vessel
is compressing the nerve. The goal of a number of surgical procedures is to
either damage or destroy the part of the trigeminal nerve that's the source of
the pain. Because the success of these procedures depends on damaging the nerve,
one side effect is facial numbness of varying degrees.
These procedures involve:
Alcohol injection. Alcohol injections under the skin of your face at the
areas of pain may offer temporary pain relief by numbing the areas for days or
months. Because the pain relief isn't permanent, you may need repeated
injections.
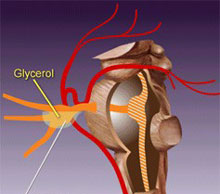 Glycerol injection. This procedure is called percutaneous glycerol
rhizotomy (PGR), Percutaneous means through the skin. Your doctor inserts a
needle into the trigeminal cistern (a small sac of spinal fluid that contains
the trigeminal nerve ganglion and part of its root). Images are made to confirm
that the needle is in the proper location. Once the location is confirmed, your
doctor injects a small amount of sterile glycerol. After 3 or 4 hours, the
glycerol damages the trigeminal nerve and blocks pain signals. Glycerol injection. This procedure is called percutaneous glycerol
rhizotomy (PGR), Percutaneous means through the skin. Your doctor inserts a
needle into the trigeminal cistern (a small sac of spinal fluid that contains
the trigeminal nerve ganglion and part of its root). Images are made to confirm
that the needle is in the proper location. Once the location is confirmed, your
doctor injects a small amount of sterile glycerol. After 3 or 4 hours, the
glycerol damages the trigeminal nerve and blocks pain signals.
Initially, PGR relieves pain. However, many people have a recurrence of pain,
and many experience mild facial numbness or tingling.
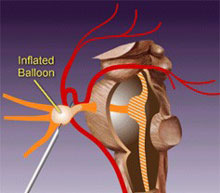 Balloon compression. In a procedure called percutaneous balloon
compression of the trigeminal nerve (PBCTN), your doctor inserts a hollow needle
through your face and into an opening in your skull. Then a thin, flexible tube
(catheter) with a balloon on the end is threaded through the needle. The balloon
is inflated with enough pressure to damage the nerve and block pain signals. Balloon compression. In a procedure called percutaneous balloon
compression of the trigeminal nerve (PBCTN), your doctor inserts a hollow needle
through your face and into an opening in your skull. Then a thin, flexible tube
(catheter) with a balloon on the end is threaded through the needle. The balloon
is inflated with enough pressure to damage the nerve and block pain signals.
PBCTN successfully controls pain in most people. Only a small number of people
experience a recurrence of pain. Most people undergoing PBCTN experience facial
numbness of varying degrees, and more than half experience nerve damage,
resulting in a temporary weakness in the muscles used to chew.
Electric current. A procedure called percutaneous stereotactic
radiofrequency thermal rhizotomy (PSR) selectively destroys nerve fibers
associated with pain. Your doctor threads a needle through your face and into an
opening in your skull. Once in place, an electrode is threaded through the
needle until it rests against the nerve root.
The electrode is positioned so that you experience numbness or pain. An electric
current is passed through the tip of the electrode until it is heated to the
desired temperature for about 70 seconds. This damages the nerve fibers and
creates an area of injury (lesion). If your pain isn't eliminated, your doctor
may create additional lesions.
PSR successfully controls pain in most people. A common side effect of this type
of treatment is mild to severe facial numbness.
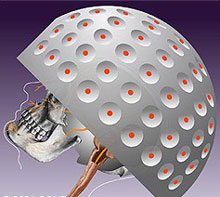 Radiation. Gamma knife radiosurgery (GKR) involves delivering single high
doses of radiation to the root of the trigeminal nerve. The radiation damages
the trigeminal nerve and eliminates the pain. GKR is successful in eliminating
pain more than half of the time. The procedure is painless and typically is done
without anesthesia. Because it's relatively new, the long-term risks of this
type of radiation are not yet known. Radiation. Gamma knife radiosurgery (GKR) involves delivering single high
doses of radiation to the root of the trigeminal nerve. The radiation damages
the trigeminal nerve and eliminates the pain. GKR is successful in eliminating
pain more than half of the time. The procedure is painless and typically is done
without anesthesia. Because it's relatively new, the long-term risks of this
type of radiation are not yet known.
Severing the nerve. Your doctor may work through a small incision to cut
the branch of the trigeminal nerve that's causing the pain as that nerve branch
leaves your skull and before it reaches your facial area.
Attacks neuralgia may stop spontaneously, become more frequent, or persist
unchanged for months or years. However, symptoms usually improve significantly
with treatment.
Microvascular decompression (MVD)
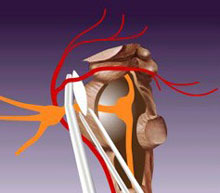 A
procedure called microvascular decompression (MVD) doesn't damage or
destroy part of the trigeminal nerve. Instead, MVD involves
relocating or removing blood vessels that have contact with the
trigeminal root and separating the root and vessels with a small
pad. A
procedure called microvascular decompression (MVD) doesn't damage or
destroy part of the trigeminal nerve. Instead, MVD involves
relocating or removing blood vessels that have contact with the
trigeminal root and separating the root and vessels with a small
pad.
During MVD, your doctor makes a small incision behind one ear. Then,
through a quarter-sized hole in your skull, part of your brain is
lifted to expose the trigeminal nerve. If your doctor finds an
artery in contact with the nerve root, he or she directs it away
from the nerve and places a pad between the nerve and the artery.
Doctors usually remove an artery that is found to be compressing the
trigeminal nerve.
MVD can successfully eliminate or reduce pain almost all of the
time, but as with every other surgical procedure for trigeminal
neuralgia, pain can recur in some people.
While MVD has a high success rate, it also carries risks. There are
small chances of decreased hearing, facial weakness, facial
numbness, double vision
and even a
stroke
or death.
|
Related Links
|
|
|
|
|
|
|







 The
trigeminal nerve is the fifth of twelve pairs of cranial nerves enervating the
face and head, and is denoted by the Roman Numeral V. It has three divisions
which enervate the forehead and eye (ophthalmic V1), cheek (maxillary V2) and
lower face and jaw (mandibular V3). The trigeminal nerves function in sensing
facial touch, pain and temperature, as well as controlling muscles used for
chewing. The trigeminal nerve functions should be distinguished from the facial
nerve (cranial nerve VII), which controls all other facial movements.
The
trigeminal nerve is the fifth of twelve pairs of cranial nerves enervating the
face and head, and is denoted by the Roman Numeral V. It has three divisions
which enervate the forehead and eye (ophthalmic V1), cheek (maxillary V2) and
lower face and jaw (mandibular V3). The trigeminal nerves function in sensing
facial touch, pain and temperature, as well as controlling muscles used for
chewing. The trigeminal nerve functions should be distinguished from the facial
nerve (cranial nerve VII), which controls all other facial movements. 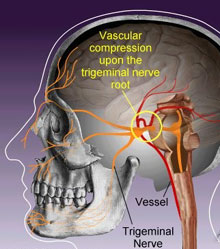 Typical
TN- This is the most common form of TN, that has previously been termed
Classical, Idiopathic and Essential TN. Nearly all cases of typical TN are
caused by blood vessels compressing the trigeminal nerve root as it enters
the brain stem.
Typical
TN- This is the most common form of TN, that has previously been termed
Classical, Idiopathic and Essential TN. Nearly all cases of typical TN are
caused by blood vessels compressing the trigeminal nerve root as it enters
the brain stem. 
 No
one test can diagnose trigeminal neuralgia. The condition must be distinguished
from other forms of facial pain that may be due to diseases of the teeth, jaw or
sinuses. Magnetic resonance imaging (MRI) or computerized tomography (CT)
scans of the brain can eliminate some causes, such as tumors, aneurysms or
multiple sclerosis, all of which can cause trigeminal neuralgia in a small
number of people.
No
one test can diagnose trigeminal neuralgia. The condition must be distinguished
from other forms of facial pain that may be due to diseases of the teeth, jaw or
sinuses. Magnetic resonance imaging (MRI) or computerized tomography (CT)
scans of the brain can eliminate some causes, such as tumors, aneurysms or
multiple sclerosis, all of which can cause trigeminal neuralgia in a small
number of people. Your
doctor may prescribe painkillers, such as paracetamol or ibuprofen.
Your
doctor may prescribe painkillers, such as paracetamol or ibuprofen.  Baclofen
(Lioresal) a muscle relaxant may be used in combination with carbamazepine or
phenytoin. Side effects include confusion, mental depression and severe
drowsiness.
Baclofen
(Lioresal) a muscle relaxant may be used in combination with carbamazepine or
phenytoin. Side effects include confusion, mental depression and severe
drowsiness.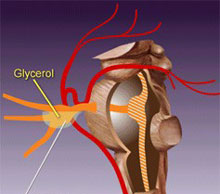 Glycerol injection. This procedure is called percutaneous glycerol
rhizotomy (PGR), Percutaneous means through the skin. Your doctor inserts a
needle into the trigeminal cistern (a small sac of spinal fluid that contains
the trigeminal nerve ganglion and part of its root). Images are made to confirm
that the needle is in the proper location. Once the location is confirmed, your
doctor injects a small amount of sterile glycerol. After 3 or 4 hours, the
glycerol damages the trigeminal nerve and blocks pain signals.
Glycerol injection. This procedure is called percutaneous glycerol
rhizotomy (PGR), Percutaneous means through the skin. Your doctor inserts a
needle into the trigeminal cistern (a small sac of spinal fluid that contains
the trigeminal nerve ganglion and part of its root). Images are made to confirm
that the needle is in the proper location. Once the location is confirmed, your
doctor injects a small amount of sterile glycerol. After 3 or 4 hours, the
glycerol damages the trigeminal nerve and blocks pain signals. 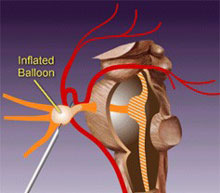 Balloon compression. In a procedure called percutaneous balloon
compression of the trigeminal nerve (PBCTN), your doctor inserts a hollow needle
through your face and into an opening in your skull. Then a thin, flexible tube
(catheter) with a balloon on the end is threaded through the needle. The balloon
is inflated with enough pressure to damage the nerve and block pain signals.
Balloon compression. In a procedure called percutaneous balloon
compression of the trigeminal nerve (PBCTN), your doctor inserts a hollow needle
through your face and into an opening in your skull. Then a thin, flexible tube
(catheter) with a balloon on the end is threaded through the needle. The balloon
is inflated with enough pressure to damage the nerve and block pain signals. 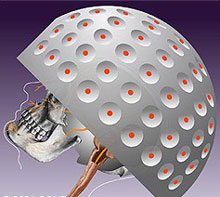 Radiation. Gamma knife radiosurgery (GKR) involves delivering single high
doses of radiation to the root of the trigeminal nerve. The radiation damages
the trigeminal nerve and eliminates the pain. GKR is successful in eliminating
pain more than half of the time. The procedure is painless and typically is done
without anesthesia. Because it's relatively new, the long-term risks of this
type of radiation are not yet known.
Radiation. Gamma knife radiosurgery (GKR) involves delivering single high
doses of radiation to the root of the trigeminal nerve. The radiation damages
the trigeminal nerve and eliminates the pain. GKR is successful in eliminating
pain more than half of the time. The procedure is painless and typically is done
without anesthesia. Because it's relatively new, the long-term risks of this
type of radiation are not yet known. 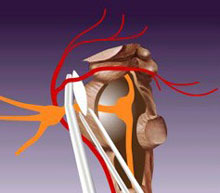 A
procedure called microvascular decompression (MVD) doesn't damage or
destroy part of the trigeminal nerve. Instead, MVD involves
relocating or removing blood vessels that have contact with the
trigeminal root and separating the root and vessels with a small
pad.
A
procedure called microvascular decompression (MVD) doesn't damage or
destroy part of the trigeminal nerve. Instead, MVD involves
relocating or removing blood vessels that have contact with the
trigeminal root and separating the root and vessels with a small
pad.