Ovarian cancer is the second most common reproductive cancer in women after endometrial cancer. Cancer occurs when cells undergo a transformation and begin to grow and multiply without normal controls. As the cells grow and multiply, they form masses called tumors. Ovarian cancer occurs when a tumor forms in one or both of a woman’s ovaries. Ovarian tumors are classified on the basis of the type of cell from which the abnormal growth originated.
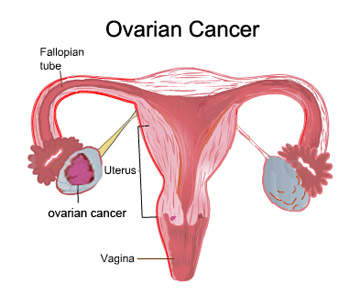
- Epithelial tumors: These tumors arise from a layer of cells that surrounds the outside of the ovary called the germinal epithelium. About 70-80% of all ovarian cancers are epithelial. These are usually found in women who have been through menopause (aged 45-70 years).
- Stromal tumors: Stromal tumors develop from connective tissue cells that help form the structure of the ovary and produce hormones. Usually, only one ovary is involved. These account for 5-10% of ovarian cancers. These tumors typically occur in women aged 40-60 years. Often, surgical removal of the tumor is the only treatment needed. If the tumor has spread, though, chemotherapy is needed.
- Germ cell tumors: Tumors that arise from germ cells (cells that produce the egg) account for about 15% of all ovarian cancers. These tumors develop most often in young women (including teenaged girls). Although 90% of women with this type of cancer are successfully treated, many become permanently infertile.
- Metastatic tumors: Only 5% of ovarian cancers have spread from other sites. The most common sites from which they spread are the colon (52%), breast (17%), stomach (10%), and pancreas (5%).
- Within these main classes are many different subtypes of tumors.
Ovarian Cancer is much more likely to be fatal than cancer of the cervix or endometrium because it is more difficult to detect at an early stage.
Stages of ovarian cancer
Ovarian Cancer is also identified by a series of i>stages. The stage describes the extent of the disease at the time of diagnosis, including tumor size and whether the cancer has spread (metastasized) to other areas of the body. The stages are commonly described as follows:
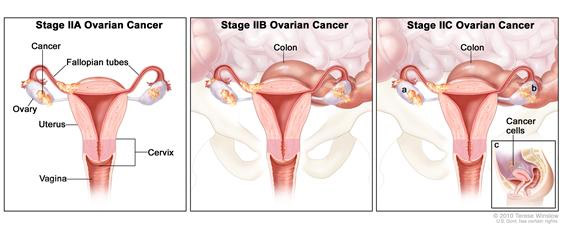
- Stage I – Growth of tumor limited to the ovaries
- Stage II – Growth of tumor in one or both ovaries
- Stage III – Tumor involving one or both ovaries with peritoneal implants outside the pelvis and/or positive retroperitoneal or inguinal lymph nodes. Superficial liver metastasis equals stage III.
- Stage IV – Growth involving one or both ovaries with distant metastases. If pleural effusion is present there must be positive cytology to allot a case to stage IV. Tumor spread inside the liver, equals stage IV.
- Recurrent/Refractory – Recurrence means that the tumor has returned after initial therapy. Refractory means that the tumor fails to respond to initial treatment.
What are the common symptoms?
Symptoms Ovarian caner has no symptoms in the early stages. The cancer is most often detected when a doctor feels an enlarged ovary during a routine pelvic examination or while he or she is investigating other problems in the reproductive tract. At more advanced stages, a woman with ovarian cancer may have vague intestinal problems, a sensation of fullness, and abdominal or pelvic pain or discomfort. (As the cancer progress, it causes fluid to build up inside the abdomen.) Often a woman’s first indication of a problem is noticing that her waistline is expanding for no apparent reasons and her clothes don’t fit. Occasionally, bleeding, like a period, may occur in a woman who has passed the menopause. At this stage, a woman may become anaemic, may lose her appetite, may lose weight and may start to feel unusually tired.
If the cancer spreads to places outside the abdomen, other symptoms may develop. For example, if the liver is involved, then the skin and the whites of the eyes may turn yellow: this is called jaundice. If the lungs are affected, then this may cause breathlessness and coughing. Ovarian cancer is a fatal condition if it is not treated.
What causes ovarian cancer and who is at risk?
Regular ovulation that is not interrupted by pregnancy or breast-feeding appears to play a major role in the development of ovarian cancer. In the process of ovulation, cells in the ovaries are continuously dividing. The constant cellular activity increases the possibility of genetic mistakes occurring in ovarian cells, which can lead to cancer.
Ovarian cancer has been linked with 3 hereditary syndromes.
- Breast-ovarian cancer syndrome
- Hereditary nonpolyposis colorectal cancer syndrome
- Site-specific ovarian cancer syndrome
The following factors increase a woman’s risk of ovarian cancer:
- Never having children- Term pregnancy (lasting the full 9 months) significantly reduces the risk of ovarian cancer. As the number of pregnancies increases, the risk of ovarian cancer decreases. Besides, Breastfeeding lowers risk of ovarian cancer, and the risk decreases with increasing duration of breastfeeding.
- Having children at an older age
- Going through menopause late (after age 55)
- Ovarian CancerHigh-Fat Diet – Ovarian Cancer has been linked to an increased amount of estrogen activity in the body. Excess fat can cause the body to retain estrogen and may convert other hormones into a form of estrogen, increasing the risks of Ovarian Cancer.
- Never having taken oral contraceptives (which block ovulation) Some studies have shown that the use of fertility drugs increases the risk of ovarian cancer, but study results have not been consistent.
- Having family history of cancer of the colon, breast, prostate, or lung
- Having a history of cancer of the breast, endometrium, or colon and rectum. There is a known inheritable genetic mutation that puts women at a higher risk for developing Ovarian Cancer. If a woman has one or more primary relatives (mother or sister) who have had Ovarian Cancer, she is three times more likely to be diagnosed with the disease herself. Genetic testing can be done on women in this “high risk” group to determine if they carry one of the gene mutations. Being a carrier of this gene does not necessarily mean that a woman has or will develop Ovarian Cancer. It simply means that a woman is at a higher risk of developing Ovarian Cancer and should be followed very closely for evidence of the disease.
- Being white- White women are much more likely to have ovarian cancer than African American women.
Diagnosis
There is no uniformly accepted test for Ovarian Cancer at this time. The ovaries are difficult to examine since they are set deep in the abdomen. Annual pelvic and rectal examinations in which the doctor feels for any abnormalities in the ovaries are the best ways to detect early signs of ovarian cancer in women with no symptoms or known risk factors. Another way to determine if a woman has Ovarian Cancer is to take a sample of ovary and abdominal tissue (Biopsy). The tissue sample is then examined under a microscope to determine if cancer cells are present.
After menopause, women who are at increased risk of ovarian cancer or who are experiencing symptoms may choose to have yearly CA_125 blood test. But the CA-125 test does not always detect ovarian cancer that is present (doctors call this is a “false negative” test result), CA-125 levels can be elevated because of non-cancerous conditions including endometriosis, fibroids, pelvic infections, pregnancy, and menstruation. Other conditions that may raise CA-125 levels are hepatitis. These factors cause positive readings in women who do not have ovarian cancer.
Vaginal ultrasound or computerised tomography (CT scanning) may be used to look at the ovaries if cancer is suspected. If the ultrasound of scan does show a tumor, surgery is required to remove the tumor and rule out cancer. Most of the time, tumors in the ovary are found to be non-cancerous. Color-flow Doppler, is another type of ultrasound test that checks the blood flow to the ovaries. An increase in blood flow to a certain area can be an indication of cancer in that region.
Culdocentesis involves the use of a needle to obtain a sample of fluid from the vaginal wall and the area surrounding the ovaries, which can then be analyzed for the presence of cancer cells.
A doctor may use laparoscopy to diagnose ovarian cancer and determine the degree to which it has spread. A flexible fibre-optic tube is inserted into the abdominal cavity by means of a small cut in the skin just below the navel. A sample of the suspected abnormal tissue, a ‘biopsy’, may be taken and sent to the laboratory for microscopic examination to determine whether this is an ovarian cancer and if so, what sort. Similarly, if fluid has accumulated in the abdomen, it can be drawn out (aspirated) through a needle and examined to see whether cancer cells are present. However, it is usually necessary to perform more extensive surgery (called exploratory laparotomy) through a larger abdominal incision to establish the diagnosis and full extent of the cancer.
Hysteroscopy- A hysteroscope is an instrument used to see inside the uterus and fallopian tube. Hysteroscopy is used to diagnose disorders such as uterine polyps and can be performed under general or local anesthesia in an outpatient clinic.
Some women at very high risk of ovarian cancer, such as those with more than one close relative (mother, daughter, aunt, or sister) with the disease, may choose to have their ovaries removed as a preventive measure. Women who make this choice usually have completed their childbearing and are nearing menopause. After surgery, they can replenish and maintain their supply of estrogen by taking hormone replacement therapy.
Treatment Options
About 80 to 85 percent of ovarian cancers start in the epithelial cells, which are cells that cover the surface of the ovaries. Epithelial ovarian cancer is most common in women over 40. Other types of ovarian cancer, including those that originate in the egg or the tissue in which the egg grows inside the ovary, tend to occur in women under 40.
Treatment depends on the type of cancer and how far it has spread. A woman’s age, her general state of health, and whether or not she has completed her family are all considerations in the choice of treatment. For example, if a young woman has a tumor in a very early stage that is confined to one ovary, her doctor may remove only that ovary to preserve her ability to have children. However, the doctor may recommend removal of her other ovary and her uterus once she has completed her childbearing.
Surgical treatment for ovarian cancer usually consists of removing the ovaries, uterus, cervix, fallopian tubes, and the omentum. Staging is performed by the surgeon (gynecologic oncologist) when the ovarian cancer is removed.
Ovarian cancer has been linked with 3 hereditary syndromes. Breast-ovarian cancer syndrome Hereditary nonpolyposis colorectal cancer syndrome Site-specific ovarian cancer syndrome
When deciding on a treatment method, doctors consider the patient’s stage of life, general health, and the size and location of any tumors. In most cases of Ovarian Cancer, a combination of surgery and either chemotherapy or radiation is used.
| surgical methods are used to treat Ovarian Cancer: | Other methods are used to treat Ovarian Cancer: |
| Oophorectomy | Chemotherapy |
| Hysterectomy | Radiation |
| Debulking | Biological Therapy |
Oophorectomy – This is the removal of one or both of the ovaries affected by the cancer.
Hysterectomy – This is the removal of the uterus and possibly the fallopian tubes to remove any tumors that have spread to these organs. This is usually done in addition to an oophorectomy.
Debulking – This procedure is used for advanced cases. The ovaries, fallopian tubes and uterus are all removed, as well as any cancer deposits the surgeon can see, in an effort to remove as many cancer cells as possible from the body. This procedure is used for advanced cases.
Other treatments:-
Chemotherapy – Chemotherapy is a systemic, or whole body, treatment, the goal of which is to kill any remaining cancer cells in the body and to keep the cancer from spreading to other organs. The drugs are typically given in cycles of a few days of treatment and then 3-4 weeks of rest, for a period of weeks or months determined by the oncologist. Drugs are administered by mouth or injection to kill the cancer cells. The drugs enter the blood stream and can, therefore, reach areas of the body where the cancer may have spread. When Ovarian Cancer is confined to the abdomen (peritoneal carcinomatosis), chemotherapy may be given directly to the abdominal lining, reducing the number of affected systems and concentrating the drug’s effects in the cancer region.
Radiation – This is the least common treatment for Ovarian Cancer compared with surgery and chemotherapy. Radiation therapy is the process in which high-energy x-rays are directed at the affected area in order to kill cancer cells. Radiation therapy is local, affecting only the area exposed to the rays. It is typically given five days per week for a period of five or six weeks.
Biological Therapy – This is a relatively new and for the most part still experimental method of cancer treatment. It involves using substances to boost the body’s own immune system responses to kill the cancer cells. In particular, monoclonal antibodies directed against ovarian cancer have been developed and are now under study.
Possible side effects from Surgical Treatmentatment
Infertility – Any surgery that removes the ovaries or uterus prevents the possibility of becoming pregnant.
Temporary pain or discomfort due to surgical incisions.
Early menopause symptoms – Common symptoms are hot flashes and vaginal dryness, and are usually treated with hormone replacement therapy. In the long term, effects of removing the ovaries include osteoporosis and increased risks of coronary artery disease.
Incontinence – Temporary incontinence or an inability to move the bowels is sometimes experienced for a short time after surgery. Click here for Kegel exercise.
The doctor may perform additional surgery to determine the extent of the cancer’s spread beyond the ovaries or, if it has spread, to take out as much of the cancer as possible. In some cases, a portion of the intestine must also be removed.
Prevention
Certain lifestyle habits can help to reduce your risk of developing Ovarian Cancer (as well as other cancers):
- Yearly gynecological exam and pelvic exam
- Exercise
- Low-fat diet
- Not smoking