In a new commentary for the journal Science, an associate vice president for research at The University of Texas at Arlington argues that emerging protein-based immunotherapy could lead to highly effective “off-the-shelf” cancer treatments for more patients.
Jon Weidanz, who also is a professor in the College of Nursing and Health Innovation at UTA, is the author of a perspective regarding the development of cancer immunotherapies.
His article, “Targeting cancer with bispecific antibodies,” will appear in the March 5 edition of Science. It evaluates the findings of three studies by researchers at Johns Hopkins University and proposes that an emerging method of protein-based immunotherapy that targets commonly occurring mutations in cancer cells or neoantigens — mutated antigens produced by tumor cells — could lead to treatments that are effective for oncology patients.
Immunotherapy, a method to treat illness by stimulating a person’s immune system, is a developing alternative to traditional cancer treatments.
“Up until recently patients were limited to four treatment options: surgery, radiation, chemotherapy and targeted therapy,” Weidanz said. “However, the holy grail has always been to develop strategies that would harness the power of the immune system to attack and destroy the cancer. With recent breakthroughs in immuno-oncology along with the new findings being published in Science, it does appear we are closing in on cancer with new immunotherapies.”
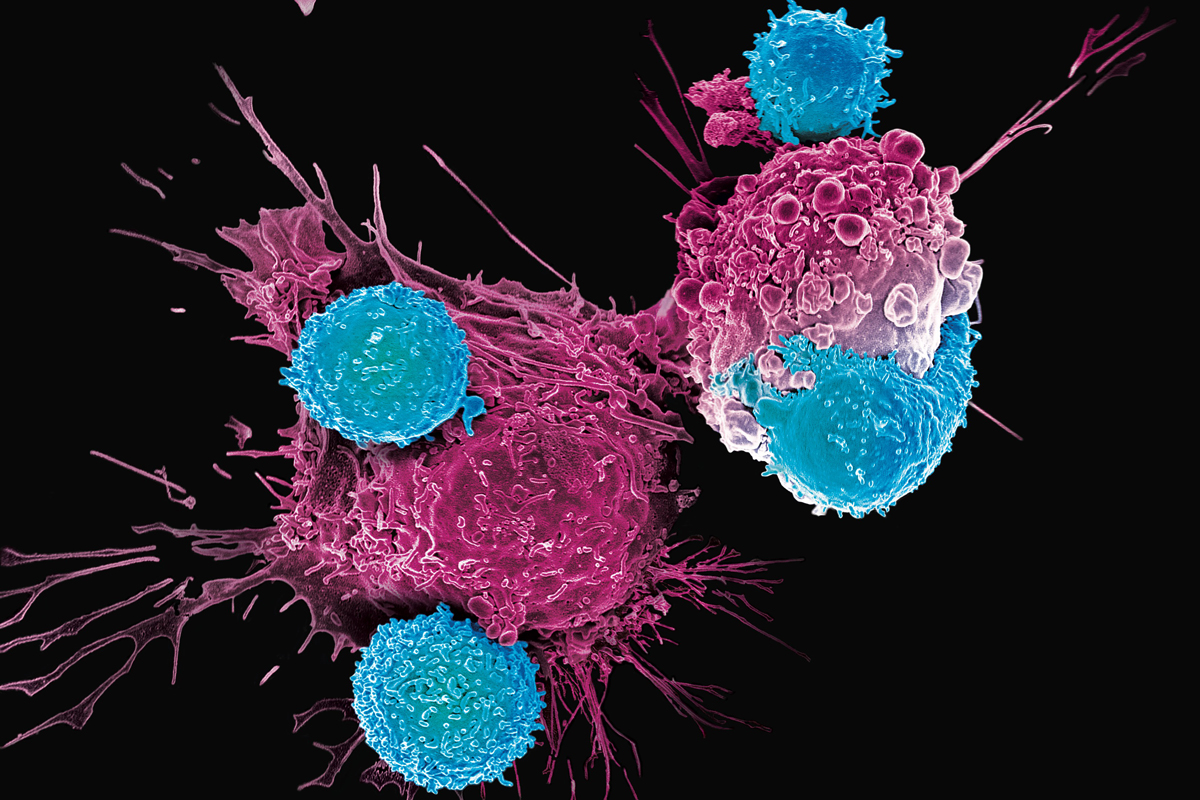
As medicine has advanced, immunologists have discovered ways to engineer a person’s T-cells, the white blood cells that fight and kill infected cells, to recognize and target cancer cells and eliminate them from the body. This approach has led to exciting advances in the field and remission in some patients. However, more work is required to make this form of T-cell therapy more broadly accessible.
Alternatively, researchers have developed approaches that stimulate the immune system without removing T-cells from the body. These “off-the-shelf” protein-based treatments, known as bispecific T-cell engaging antibodies, have proven effective in treating patients with acute lymphoblastic leukemia, a type of blood cancer.
“The ideal is to create protein molecules that have two arms. One arm can recognize the cancer cell and bind to it. The other arm binds to T-cells,” Weidanz said. “The protein drug then brings the T-cells into proximity with the tumor cells, which activate the T-cells to destroy the tumor cells.”
These two-armed, or bispecific, proteins would avoid healthy cells while destroying cancer cells. Weidanz argues that this method of protein-based immunotherapy could make a difference. The key comes down to the unique targets expressed by the cancer cells that the bispecific protein drug recognizes. Bispecific antibodies could bind to particular neoantigen targets found on tumor cells and recruit T-cells to destroy the cancer.
“The beauty of bispecific proteins is that you could manufacture those proteins and put them on the shelf as an immunotherapy agent,” Weidanz said. “If a doctor sees that a patient’s cancer expresses the neoantigen target, they could be treated immediately. It’s still a personalized medicine, but would not require engineering T-cells.”
An expert in immunology, Weidanz has more than 30 years of experience in biotechnology research with an emphasis on immunotherapy, especially related to oncology and product development to diagnose and treat cancer. His research lab at UTA investigates how the immune system identifies malignant cells with the goal of designing treatments that boost immune cells’ ability to destroy cancerous cells.
“Dr. Weidanz’s substantial expertise in the field of immunology will lead us into the next generation of cancer management,” said James Grover, interim vice president of research. “The developments of his lab and those of his many talented colleagues across the nation make this a pivotal moment in the history of a devastating disease.”
Weidanz said immunotherapy holds the promise of transforming cancer into a more manageable condition with better prognoses for patients.
“We are getting to a point where we will be able to make cancer more of a chronic disease,” Weidanz said. “Now, we look at five-year survival. Maybe we can start looking at 15- or 20-year survival readouts because we’re able to manage the disease with immunotherapies that are being developed. It’s a very exciting time.”