A European consortium of epilepsy researchers has reported the discovery of a new gene involved in severe childhood epilepsy. Using a novel combination of technologies, including trio exome sequencing of patient/parental DNA and genetic studies in the tiny larvae of zebrafish, the EuroEPINOMICS RES consortium found that mutations in the gene CHD2 are responsible for a subset of epilepsy patients with symptoms similar to Dravet syndrome — a severe form of childhood epilepsy that is in many patients resistant to currently available anti-epileptic drugs.
The discovery of CHD2’s role in epilepsy offers new diagnostic tools for families and clinicians of children with Dravet syndrome and related genetic epilepsies. In addition, the creation of a zebrafish model for CHD2 encephalopathy may facilitate the discovery of new drugs that can treat patients with this form of epilepsy.
Dravet syndrome is a severe genetic epilepsy with onset during infancy, with initial seizures often triggered by fever. For most Dravet patients these seizures cannot be treated adequately with currently available anti-epileptic drugs, and therefore the syndrome is classified as pharmacoresistant. Dravet patients usually develop moderate to severe cognitive delays and some features of autism, and are at increased risk of SUDEP (sudden unexplained death in epilepsy). Approximately 80% of Dravet patients have mutations in the gene SCN1A which encodes the Nav1.1 sodium channel, however for the remaining 20% of patients the underlying genetic cause has yet to be determined.
To identify novel genes involved in Dravet Syndrome and other genetic epilepsies, epilepsy clinicians and human geneticists across Europe recently initiated the EuroEPINOMICS RES (Rare Epilepsy Syndromes) consortium. In 2011, the EuroEPINOMICS RES consortium was awarded €2,37 million in funding from the national funding agencies participating in the European Science Foundation program to systematically search for novel genes for seizure disorders.
As part of these ongoing research activities, the DNA of Dravet patients without SCN1A mutations was analyzed by trio exome sequencing, which searches across the active parts of the genome for de novo mutations that have arisen in these patients (de novo mutations are DNA copying errors that occur in the parents’ gametes or in the fertilized egg or embryo, resulting in the afflicted family member being the first person in their family to have this genetic condition). In a group of 9 such patients, this analysis of their DNA (and the DNA of their parents) resulted in the identification of 2 patients with de novo mutations in CHD2, which stands for chromodomain helicase DNA binding protein 2. A third patient with a CHD2 mutation was subsequently identified as well.
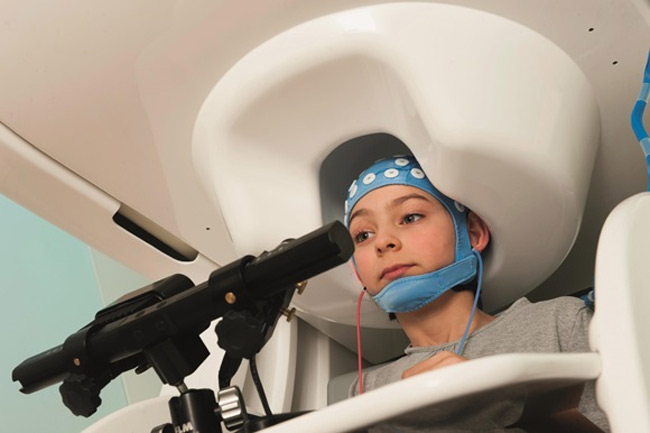
To confirm that mutations in CHD2 cause the epilepsy observed in these patients, the same gene was then functionally analyzed in the tiny larvae of zebrafish, which have emerged in the last decade as a powerful animal model for the study of epilepsy. In the case of CHD2, scientists collaborating with the EuroEPINOMICS RES consortium used antisense technology to rapidly generate zebrafish larvae with a partial loss of function of this gene, and were then able to detect epileptic seizures in these animals using electrographic analysis (this method is very similar to electroencephalography, or EEG, which is used to analyze seizures in humans).
The genetic analysis was led by Peter De Jonghe, head of the Neurogenetics Group of the VIB Department of Molecular Genetics at the University of Antwerp (Antwerp, Belgium) and the epilepsy genetics group in Kiel, headed by Ingo Helbig (Dept. of Neuropediatrics, University of Kiel, Germany). Peter De Jonghe: “This research reinforces our belief that trio sequencing enables us to unravel the genetic background of syndromes which occur spontaneously. Previously, investigations into the genetic causes of syndromes such as Dravet Syndrome were not feasible. These types of investigations were only possible by screening large families and seeing how a disorder was passed along. But in disorders such as Dravet Syndrome, this did not work since the children were so seriously ill that they themselves never went on to have their own children. So this new technology also opens up new perspectives in the search for the genetic background of many disorders.”
Ingo Helbig adds that “the epileptic encephalopathies pose a major clinical problem as most children have treatment-resistant epilepsy, intellectual disability and many other medical issues. We hope that identifying the underlying genetic cause will help us find better treatment options for the affected patients. In the past, we were not able to identify the reason why children have severe epilepsy. The discovery of CHD2 as the culprit gene in a subset of children with epileptic encephalopathy is a major step for us.”
The zebrafish research was led by Camila Esguerra of the Laboratory for Molecular Biodiscovery of University of Leuven (Leuven, Belgium). She commented: “Our previous research to validate zebrafish as a model for epilepsy put us in a good position to be able to help the EuroEPINOMICS consortium investigate the function of CHD2. The zebrafish larva is an ideal model to study genes involved in epilepsy, and the methods necessary for such studies are now well-established in our laboratory. Looking forward, our zebrafish models of pharmacoresisant epilepsy are well-suited for large-scale pharmacological screens to find new anti-epileptic drugs.”
The Dravet Syndrome Foundation EU (DSF-EU, Madrid, Spain) is a patient organization dedicated to finding a cure for Dravet Syndrome, and also works to promote awareness of the disease and to help families of Dravet patients. Julian Isla, Executive Director of DSF-EU, stated: “One of the most important things for patients with genetic disorders and their families is to be able to give a name to the gene causing their disease. When it comes to Dravet syndrome, the genes responsible for up to 20% of the cases are still unknown. The discovery that mutations in CHD2 cause a Dravet-like syndrome means some of these patients will now have access to better genetic diagnosis and therefore provide much-needed answers to these families. Importantly, the development of a new animal model for Dravet syndrome based on reduced CHD2 expression might help to find effective treatments that could improve the lives of thousands of people suffering from Dravet syndrome and perhaps other genetic epilepsies.”
The study done by VIB (the Flanders Institute for Biotechnology).