What is Multiple sclerosis?
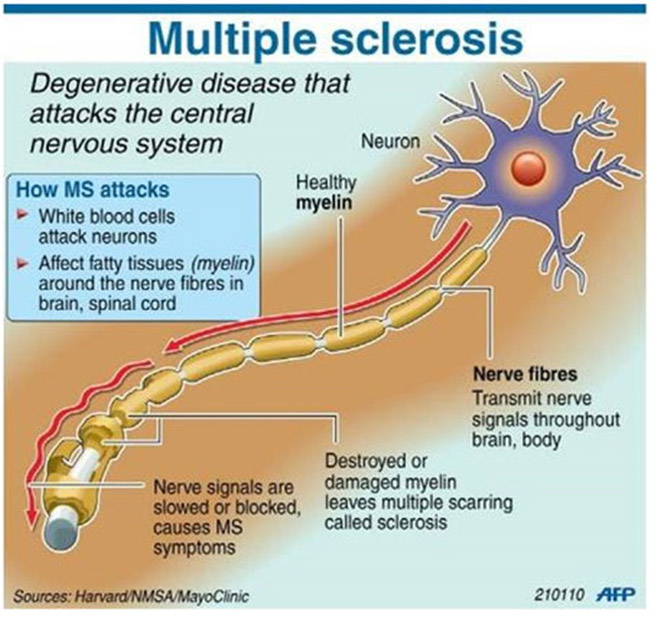
A progressive disease of nerves in the brain and spinal cord causing weakness and problems with sensation and vision
Multiple sclerosis (MS) is the most common nervous system disorder affecting young adults. In this condition, nerves in the brain and spinal cord are progressively damaged, causing a wide range of symptoms that affect sensation, movement, body functions, and balance. Specific symptoms may relate to the particular areas that are damaged and vary in severity between individuals. For example, damage to the optic nerve may cause blurred vision. If nerve fibres in the spinal cord are affected, it may cause weakness and heaviness in the legs or arms. Damage to nerves in the brain stem, the area of the brain that connects to the spinal cord, may affect balance.
In many people with MS, symptoms occur intermittently and there may be long periods of remission. However, some people have chronic (long-term) symptoms that gradually get worse.
|
AGE |
Usually develops between the ages of 20 and 40. |
|
GENDER |
More common in females |
|
GENETICS |
Sometimes runs in families |
|
LIFESTYLE |
Stress and heat may aggravate symptoms |
There are different types of MS.
-
Benign MS- this form or stage of MS does not worsen with time and there is no permanent disability or disease progression.
-
Relapsing-remitting MS- symptoms last for days or weeks and then clear up for months or even years. However, some symptoms may eventually persist between the attacks. In this form or stage of MS there are sporadic attacks (exacerbations, relapses), during which new symptoms appear and/or existing ones become more severe.
-
Chronic-progressive MS, in which there is a gradual worsening of symptoms with no remission. A person with relapsing - remitting MS may go on to develop chronic-progressive MS. By now, more CNS tissue has now been destroyed.

Symptoms may occur singly in the initial stages and in combination as the disorder progresses. They may include :
-
Visual Disturbances
Blurring of vision, double vision (diplopia), optic neuritis, involuntary rapid eye movement, (rarely) total loss of sight.
-
Altered Sensations
Tingling, numbness (paresthesia), a burning feeling in an area of the body or other indefinable sensations
-
Fatigue
A debilitating kind of general fatigue that is unpredictable and out of proportion to the activity; fatigue is one of the most common (and one of the most troubling) symptoms of MS
-
Weakness
weakness and feeling of heaviness in the legs or arms.
-
Balance and Coordination Problems
Loss of balance, tremor, unstable walking (ataxia), dizziness (vertigo), clumsiness of a limb, lack of coordination.
-
Abnormal Speech
Slowing of speech, slurring of words, and changes in rhythm of speech.
-
Cognitive Function
Short-term memory problems and difficulty concentrating and thinking, but typically not severe enough to seriously interfere with daily functioning for most people with MS. Judgment and reasoning may also be affected. Stress and heat sometimes make symptoms worse. About half of the people who have MS find it hard to concentrate and experience memory lapses.
-
Spasticity
Altered muscle tone can produce spasms or muscle stiffness, which can affect mobility and walking
-
Difficulty in Swallowing (dysphagia)
-
Bladder and Bowel Problems
The need to pass urine frequently and/or urgently, incomplete emptying or emptying at inappropriate times, constipation, and loss of bowel control

-
Depression is common.
-
Pain
Facial pain and muscle pains. Later in the course of the disease, some people with muscle weakness develop painful muscle spasms.
-
Sexuality and Intimacy
Impotence, diminished arousal and loss of sensation
- Eventually damage to myelin covering nerves in the spinal cord may cause partial paralysis, and an affected person may need a wheelchair.
Though these are a few of the symptoms commonly associated with MS, not all people with MS will experience all of them. Most will experience more than one symptom, however. There is no typical case of MS. Each is unique.
Scientific research seems to show that the causal factors of immunological, environmental, genetic, and viral, in various combinations, are the most likely reason for MS.
Immunology
MS is an autoimmune disorder, in which the body's immune
system attacks its own tissues, in this case those of the nervous system.
Many nerves in the brain and spinal cord are covered by a protective insulating
sheath of material called myelin. In MS, small areas of myelin are
damaged, leaving holes in the sheath, a process known as demyelination.
Once the myelin sheath has been damaged, impulses cannot be conducted normally
along nerves to and from the brain and spinal cord. At first, the damage
may be limited to only one nerve, but myelin covering other nerves may become
damaged over time. Eventually, damaged patches of myelin insulation are
replaced by scar tissue.
Environment
The geographic location of a young person can
be a significant factor (2X) in the probability of MS occurring. An unusual
characteristic of MS worldwide is that it occurs in the general population at
roughly twice the rate for those living above approximately the 40 latitude
than for those living below the 40 latitude.
Genetics
MS is not a hereditary disease; however, the genetic component, or
marker, for people who are predisposed to develop MS can be shown, and some
probabilities can be calculated. The exact mechanism of action that causes this
genetic marker to increase the probability that the myelin of a patient will be
sensitive to attack by
immune system cells is not known. Scientists believe that
certain "unlucky" combinations of genes may significantly increase a person's
chance of developing MS. Genetic factors that are common among immediate family
members such as parents, brothers, or sisters can increase the risk of
developing MS by severalfold.
Viruses
Some viruses are known to cause demyelination and inflammation, so the
possibility that a viral factor is a trigger in the development of MS is
considered by some researchers to be significant.
Doctors use two basic rules to determine if a
patient has MS:
-
A patient must
experience two separate attacks at least one month apart-an attack, also
called a flare or relapse (exacerbation), is the sudden appearance (lasting at
least 24 hours) of a classic MS symptom-and
- There must be detectable damage to the myelin of the CNS. There must be a history of myelin damage. It must have occurred more than once and must not have a causal connection with other demyelination diseases.
Medical History:
Clinical examination includes a detailed review of the five
senses, mental and cognitive function, language and speech function, family
history, sex, emotional factors, geographic data, and the age when the symptoms
first appeared. The medical history of MS patients should include information on
the following: date and type of symptoms, medications, allergies, history of
surgery or trauma, family history (MS positive), sexual function, bowel and
bladder habits, exposure to environmental hazards such as chemicals, and foreign
travel with the possibility of exposure to exotic diseases.
Neurological Examination:
If you are having visual problems, such as blurred vision, you may be
referred to an ophthalmologist, who will assess the optic nerve for optic
neuritis, which is commonly
affected in the early stages of the disorder.
Evoked potential testing is electrical diagnostic testing used to determine if there is a slowing of message transmission in various parts of the brain. These tests can often pinpoint nerve sheath (myelin) scarring not found in neurological examination. Normally, the Brain's reaction to such stimuli is almost instantaneous. DeMyelination or a Lesion in the Nerve Pathway cause a conduction delay and the response time will be much slower than normal (Longer Latency Time).
You will probably also have an imaging test of the brain, such as MRI ,
to see if there are areas of demyelination. MRI
testing can be used to track and predict the progression of MS once the presence
of the disease has been detected. MRI testing is a sophisticated enough
neuropsychologic tool to detect demyelination that is associated with cognitive
function. Bear in mind that a normal MRI does not ensure that a person does not
have MS. About five percent of MS patients have normal MRIs, according to the
National Multiple Sclerosis Society.
Your doctor may arrange for a lumbar puncture (Spinal Tap), a procedure in which a small amount of the fluid that surrounds the spinal cord is removed for microscopic analysis. Abnormalities in this fluid may confirm the diagnosis.
Other testing can determine the presence of MS when other clinical data are not conclusive. These tests may include blood testing used to determine the presence of a group of diseases known as collagen-vascular disease, Lyme disease, and AIDS.

There is no cure for MS, but if you have relapsing-remitting MS, interferon beta may help to lengthen remission periods and shorten the length of attacks. Your doctor may also prescribe corticosteroids to shorten the duration of relapse. However, at present, there is no specific treatment to halt the progression of chronic-progressive MS. The "ABC drugs (Avonex ,Betaseron and Copaxone)," have revolutionized the way relapsing-remitting MS is treated. The ABC drugs do not stop MS entirely or cure it, but they do reduce the frequency and intensity of attacks and slow the progress of damage.
Most recently (March 2002), the U.S. Food and Drug Administration (FDA) approved a third form of interferon called Rebif. Like the ABC drugs, it is indicated for the treatment of patients with relapsing forms of MS to decrease the frequency of clinical exacerbations and delay the accumulation of physical disability. Like Avonex, Rebif is the beta-1a form of the human protein interferon. Additional information about Rebif is available from the manufacturer's Web site: http://www.rebif.com .
Many of the more common symptoms that occur in all types of MS can be relieved by drugs. For example, your doctor may treat muscle spasms with a muscle relaxant. For example, baclofen (Lioresal) and tizanidine (Zanaflex) are antispasticity medications often prescribed to relieve muscle spasms, cramping, and tightness of muscles in MS patients. Each has varying side effects in varying degrees; however, your health care professional should be able to find one that provides comfort and relief for almost any symptom you have.
Similarly, incontinence can often be improved by drugs that affect bladder control. Although currently unapproved by the FDA for MS patients, a growing number of health care providers now consider use of the botulinum toxin Botox as an effective short-term treatment option for certain types of MS-related problems, such as muscle stiffness and urinary problems, when first-line treatment is ineffective.
Problems in getting an erection may be helped by a drug treatment such as sildenafil.
If you have mobility problems, your doctor may arrange for you to have physiotherapy. Physical therapy usually focuses on walking (including using ambulatory aids correctly), balance and stability in standing, maintaining range of motion and functional strengthening.
Occupational therapy may make day-to-day activities easier. Some programs also include techniques to improve memory and concentration. The American Occupational Therapy Association (AOTA) and the American Physical Therapy Association (APTA) provide referrals to specialists and information on MS-related issues as well as other conditions. Visit their Web sites for more information: http://www.aota.org and http://www.apta.org.
Lifestyle Modifications
If you are diagnosed with MS, you and your family will need time and
possibly counseling to come to terms with the disorder.
- You should minimize stress in your life and avoid exposure to high temperatures if heat tends to make your symptoms worse.
- Regular, gentle exercise, such as swimming, will help to keep your muscles strong without the risk of overstraining them. Exercise can be therapeutic and is at least as important for women with MS as for other women. If you have MS, the last thing you want is to develop other health problems - such as obesity, diabetes or heart disease. People with MS, however, should not "go for the burn" during exercise because overheating can trigger symptoms and worsen fatigue. Some women with MS enjoy exercising in a cool pool, but others find that the bother of driving and changing twice is too fatiguing. A physical therapist can help you design an appropriate exercise program.
Things you can do at home to manage fatigue and/or limited mobility include:
* De-cluttering your living areas.
* Dividing household tasks more equitably with family members.
* Simplifying tasks like cooking so they are less stressful - for example, cook more frozen vegetables, or freeze individual servings of a meal, so you can give yourself time off from meal preparation.
* Making tasks less fatiguing - for example, put a table and chair in the kitchen so you can sit while cutting or stirring.
* Identifying and abiding by your priorities. If it's important for you to continue working, take some shortcuts with household tasks, or eliminate some of them.
No matter how much you exercise, how healthful your diet is or how well you take care of yourself, there is no way to prevent multiple sclerosis (MS). It affects people randomly. But it also is somewhat manageable. If detected early, new medications (see discussion of the "ABC" drugs" in the Treatment section at this site) may slow the progress of the disease and the severity of symptoms.
