|
|
Hydrosalpinx
Hydrosalpinx, derived from Greek, literally means �water tube�.
 A
hydrosalpinx is a fallopian tube that is filled with fluid. Injury to the end of
the fallopian tube, the ampulla, and its delicate fingers, the fimbria, causes
the end of the tube to close. Glands within the tube produce a watery fluid that
collects within the tube, producing a sausage shaped swelling that is
characteristic of hydrosalpinx. A
hydrosalpinx is a fallopian tube that is filled with fluid. Injury to the end of
the fallopian tube, the ampulla, and its delicate fingers, the fimbria, causes
the end of the tube to close. Glands within the tube produce a watery fluid that
collects within the tube, producing a sausage shaped swelling that is
characteristic of hydrosalpinx.
It is a common type of tubal problem that causes
infertility. Nearly half of all couples who suffer from infertility have a
female-related cause...
Causes - The tubes are prone to injury. The fimbria are the delicate
fingers that extend from the funnel-shaped end of the fallopian tube to the
ovary. The fimbria actively search out the egg after it is released, or
ovulated, and carry the egg to the waiting sperm within the fallopian tube. The
fimbria are lined with delicate cells that contain the actively moving hair-like
cilia, which move the eggs and sperm together. With injury, not only are the
fimbria themselves injured and fused together, but also the delicate lining
cells are lost. Fluid collects within the closed tube. A normally rich and
supportive tubal environment becomes the dead sea of the hydrosalpinx.
The infection and/or pelvic adhesions (scar tissue)
that causes hydrosalpinx can result from any number of
factors, including:
-
Gonorrhea - a curable sexually transmitted
infection (STI) caused by a bacterium called
Neisseria gonorrhoeae.
-
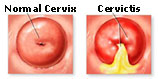 Chlamydia
- a common sexually transmitted disease (STD) caused
by the bacterium, Chlamydia trachomatis, which can
damage a woman�s reproductive organs. Chlamydia
- a common sexually transmitted disease (STD) caused
by the bacterium, Chlamydia trachomatis, which can
damage a woman�s reproductive organs.
-
Other sexually transmitted diseases
-
Having a baby
-
Having an abortion
-
Having an IUD
inserted.
|
|
 Hydrosalpinx
is a result of injury to the tube, usually from an infection. The classic causes
of hydrosalpinx are chlamydia and gonorrhea, which can run undetected for years,
slowly injuring and destroying the delicate fimbria. IUDs, endometriosis, and
abdominal surgery sometimes are associated with the problem. As a reaction to
injury, the body rushes inflammatory cells into the area, and inflammation and
later healing result in loss of the fimbria and closure of the tube. These
infections usually affect both fallopian tubes, and although a hydrosalpinx can
be one-sided, the other tube on the opposite side is often abnormal. By the time
it is detected, the tubal fluid usually is sterile, and does not contain an
active infection. Hydrosalpinx
is a result of injury to the tube, usually from an infection. The classic causes
of hydrosalpinx are chlamydia and gonorrhea, which can run undetected for years,
slowly injuring and destroying the delicate fimbria. IUDs, endometriosis, and
abdominal surgery sometimes are associated with the problem. As a reaction to
injury, the body rushes inflammatory cells into the area, and inflammation and
later healing result in loss of the fimbria and closure of the tube. These
infections usually affect both fallopian tubes, and although a hydrosalpinx can
be one-sided, the other tube on the opposite side is often abnormal. By the time
it is detected, the tubal fluid usually is sterile, and does not contain an
active infection.
Not only does a hydrosalpinx cause infertility, it can also reduce the success
rate of fertility treatment, even those treatments that bypass the fallopian
tubes. The blocked tube can communicate with the uterus, and the fluid in the
tube can be expressed out of the tube into the uterus. This fluid is probably
somewhat toxic to early embryo development, and certainly provides an
unfavorable environment. The large volume of the fluid flow back into the uterus
and can produce enough flow that embryos find it difficult to attach, since they
have no ability to move against the tide. Fertility drugs may cause the fluid to
build up in the tube, since the tubes are responsive to the ovarian hormones
produced during fertility drug therapy.
Complications - Hydrosalpinx can be hazardous during fertility evaluation
and treatment, since it is prone to re-infection. Hysterosalpingogram is a
particular problem, since the dye can inadvertently introduce bacteria into the
tubes, and a serious infection can result. Fertility procedures like
insemination and embryo transfer can cause similar problems. Infection in a
hydrosalpinx, salpingitis, can be a serious surgical emergency and result in
hospitalization.
Evaluation - Hydrosalpinx can be evaluated with several maneuvers:
-
 The
Hysterosalpingogram (HSG) is a procedure in which dye is placed through
the cervix and into the uterus and fallopian tubes. An X-ray picture then
reveals the outline of the uterus and tubes. A hydrosalpinx appears as a
large-sausage-shaped dilation of the tubes. The folds that are present
inside the tube disappear and a flat bulbous shape is seen. Dye does not
spill out of the tube. The
Hysterosalpingogram (HSG) is a procedure in which dye is placed through
the cervix and into the uterus and fallopian tubes. An X-ray picture then
reveals the outline of the uterus and tubes. A hydrosalpinx appears as a
large-sausage-shaped dilation of the tubes. The folds that are present
inside the tube disappear and a flat bulbous shape is seen. Dye does not
spill out of the tube.
-
 Ultrasound
uses sound waves to image the tubes, and is somewhat safer than HSG and more
comfortable. The best view, most of the time, is obtained with a vaginal
ultrasound probe. A normal fallopian tube is usually not visible; a
hydrosalpinx appears as a characteristic sausage-shaped fluid collection
between the ovary and fallopian tube. The wall of the hydrosalpinx is often
thick and flat. Ultrasound provides a quick and painless screen of the
pelvic organs and is an excellent first assessment of the tubes. Ultrasound
uses sound waves to image the tubes, and is somewhat safer than HSG and more
comfortable. The best view, most of the time, is obtained with a vaginal
ultrasound probe. A normal fallopian tube is usually not visible; a
hydrosalpinx appears as a characteristic sausage-shaped fluid collection
between the ovary and fallopian tube. The wall of the hydrosalpinx is often
thick and flat. Ultrasound provides a quick and painless screen of the
pelvic organs and is an excellent first assessment of the tubes.
-
 Laparoscopy
is another means of assessing the tubes, but is generally used only for
treatment and not for assessment. In laparoscopy, a small television camera
is introduced through the belly button. The pelvic organs can be visualized
on a television screen. It has been said that physicians with expertise at
video games excel at the hand-eye coordination required to perform these
procedures! Laparoscopy is the gold standard test for evaluation, since
looking at the fallopian tubes will usually provide the best view of their
anatomy. Laparoscopy
is another means of assessing the tubes, but is generally used only for
treatment and not for assessment. In laparoscopy, a small television camera
is introduced through the belly button. The pelvic organs can be visualized
on a television screen. It has been said that physicians with expertise at
video games excel at the hand-eye coordination required to perform these
procedures! Laparoscopy is the gold standard test for evaluation, since
looking at the fallopian tubes will usually provide the best view of their
anatomy.
Diagnostic tests such as ultrasound and HSG are not 100% accurate, and can
be misleading, sometimes missing significant tubal disease, and sometimes
showing abnormal results when the tubes are actually quite normal.
Laparoscopy usually will confirm the diagnostic tests, but can show that
tubes that were thought to be normal actually have significant disease, and
vice versa. The risks of anesthesia and surgery dictate that laparoscopy is
used for definitive therapy, rather than as a diagnostic test.
Treatment :
 In
vitro fertilization is the ultimate fertility therapy. The ability to
optimize fertilization rates, place embryos into their correct location, and
provide excellent hormonal support to the early developing embryo have vastly
improved success rates over the last few years. In patients with hydrosalpinx,
the fallopian tubes can be bypassed, since eggs are taken out of the ovary,
fertilized in the lab, and transferred back into the uterus. A hydrosalpinx can
be repaired, but with improving success rates from in vitro fertilization,
should it be? In
vitro fertilization is the ultimate fertility therapy. The ability to
optimize fertilization rates, place embryos into their correct location, and
provide excellent hormonal support to the early developing embryo have vastly
improved success rates over the last few years. In patients with hydrosalpinx,
the fallopian tubes can be bypassed, since eggs are taken out of the ovary,
fertilized in the lab, and transferred back into the uterus. A hydrosalpinx can
be repaired, but with improving success rates from in vitro fertilization,
should it be?
 Hydrosalpinx
can be repaired in carefully selected cases, but pregnancy rates remain rather
low. Hydrosalpinx can be treated laparoscopically, a procedure known as
neosalpingostomy. In neosalpingostomy, an incision is made in the end of the
hydrosalpinx and the edges of the incision are folded or flowered back, leaving
an open tube. Unfortunately, the tube often closes back up, and the hydrosalpinx
has a high recurrence rate. Hydrosalpinx
can be repaired in carefully selected cases, but pregnancy rates remain rather
low. Hydrosalpinx can be treated laparoscopically, a procedure known as
neosalpingostomy. In neosalpingostomy, an incision is made in the end of the
hydrosalpinx and the edges of the incision are folded or flowered back, leaving
an open tube. Unfortunately, the tube often closes back up, and the hydrosalpinx
has a high recurrence rate.
A small hydrosalpinx is the most successfully repaired. Since pregnancy
requires six months to a year after surgery, younger women with relatively
healthy ovaries and eggs, and lots of time, tend to have the best success rates.
Women with a large hydrosalpinx and those in older age groups do not benefit
from surgical repair.
A hydrosalpinx can have adverse effects on pregnancy rates with in vitro
fertilization. As success rates with in vitro fertilization have improved
dramatically over the past few years, surgical repair of the fallopian tubes
holds less appeal. Indeed, the concerns over re-infection of a hydrosalpinx and
problems with fluid build-up with fertility drug therapy have raised the stakes
for a hydrosalpinx. Removal of a damaged tube reduces the risk of complications
of therapy and improves success rates with in vitro
fertilization techniques.
 Repair
can be done in carefully selected young patients with minimal damage to their
tubes, but should not be attempted with a large hydrosalpinx in an older woman.
In these patients, the tube should be removed, via laparoscopic salpingectomy.
Salpingectomy is an easy procedure that takes less than an hour. The risks with
an experienced surgeon are low, and the benefits substantial. It is important to
choose an experienced surgeon, since considerations of safety and preservation
of the ovarian blood supply with improvement to later pregnancy rates require
judgment and experience. Repair
can be done in carefully selected young patients with minimal damage to their
tubes, but should not be attempted with a large hydrosalpinx in an older woman.
In these patients, the tube should be removed, via laparoscopic salpingectomy.
Salpingectomy is an easy procedure that takes less than an hour. The risks with
an experienced surgeon are low, and the benefits substantial. It is important to
choose an experienced surgeon, since considerations of safety and preservation
of the ovarian blood supply with improvement to later pregnancy rates require
judgment and experience.
Microsurgical salpingostomy is performed by
creating a small opening in the remaining end of the
fallopian tube with a microsurgical needle electrode.
The newly created opening is then enlarged and gently
folded back like the petals of a flower to allow the
internal endothelial lining to emerge and extend over
the opened tubal end. Since healthy tubal endothelium is
covered with cilia - the hairline projections that beat
in coordinated waves - the new tubal opening or ostium
can capture an egg as it is released from the ovary and
propel it into the tube just as the fimbrial end of the
tube does normally. Fine sutures are carefully placed
around the circumference of the folded back end of the
fallopian tube and an adhesion barrier is gently placed
over it to prevent scar formation.
|
|
Hydrosalpinx is a classic fertility problem that prevents embryos from reaching
the uterus and limits pregnancy rates. It can interfere with fertility therapy
and cause problems for in vitro fertilization. Fortunately, excellent methods
are available to manage the hydrosalpinx.
Related Links
|
|
|
|
|









