For World Hepatitis Day 2022, WHO focuses on the theme “Bringing hepatitis care closer to you” and calls for simplified service delivery of viral hepatitis services, bringing care closer to communities.
Hepatitis A is a vaccine-preventable liver infection caused by the hepatitis A virus (HAV). Almost everyone recovers fully from hepatitis A with lifelong immunity. However, a very small proportion of people infected with hepatitis A could die from fulminant hepatitis.
Mode of Transmission
Hepatitis A virus (HAV) is a virus that can be found in the gut of people and some animals.
The virus is transmitted primarily by the faecal-oral route; that is when an uninfected person ingests food or water that has been contaminated with the faeces of an infected person. In families, this may happen through dirty hands when an infected person prepares food for family members. Waterborne outbreaks, though infrequent, are usually associated with sewage-contaminated or inadequately treated water.
The virus can also be transmitted through close physical contact (such as oral-anal sex) with an infectious person, although casual contact among people does not spread the virus.
Symptoms
The incubation period of hepatitis A is usually 14–28 days.

Symptoms range from mild to severe and can include fever, malaise, loss of appetite, diarrhoea, nausea, abdominal discomfort, dark-colored urine, and jaundice (yellowing of the eyes and skin). Not everyone who is infected will have all the symptoms.
Adults have signs and symptoms of illness more often than children. The severity of disease and fatal outcomes are higher in older age groups.
Infected children under 6 years of age do not usually experience noticeable symptoms, and only 10% develop jaundice. Hepatitis A sometimes relapses, meaning the person who just recovered falls sick again with another acute episode. This is normally followed by recovery.
Who is at risk of Hepatitis A?
Anyone who has not been vaccinated or previously infected can get infected with the virus. In areas where the virus is widespread (high endemicity), most hepatitis A infections occur during early childhood. Risk factors include:
- poor sanitation
- lack of safe water
- living in a household with an infected person
- being a sexual partner of someone with acute hepatitis A infection
- use of recreational drugs
- sex between men
- traveling to areas of high endemicity without being immunized.
Diagnosis
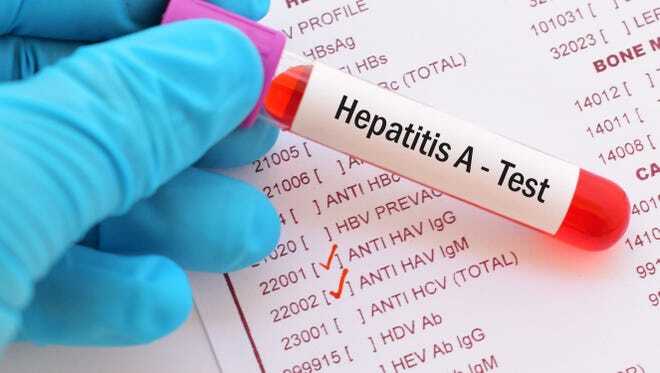
Cases are not clinically distinguishable from other types of acute viral hepatitis. Specific diagnosis is made by the detection of HAV-specific immunoglobulin G (IgM) antibodies in the blood. Additional tests include reverse transcriptase-polymerase chain reaction (RT-PCR) to detect the hepatitis A virus RNA and may require specialized laboratory facilities.
Treatment
There is no specific treatment for the disease. Recovery from symptoms following infection may be slow and can take several weeks or months. It is important to avoid unnecessary medications. Acetaminophen, paracetamol, and medication against vomiting should be avoided.
Hospitalization is unnecessary in the absence of acute liver failure. Therapy is aimed at maintaining comfort and adequate nutritional balance, including the replacement of fluids that are lost from vomiting and diarrhoea.
Prevention
Improved sanitation, food safety, and immunization are the most effective ways to combat hepatitis A.

The spread of infection can be reduced by:
- adequate supplies of safe drinking water
- proper disposal of sewage within communities
- personal hygiene practices such as regular handwashing before meals and after going to the bathroom.
- Avoid sharing food, cutlery, and drinks with other people
- Avoid eating raw or undercooked shellfish
- When traveling to places with poor sanitation, drink bottled water and avoid food that might have been prepared using contaminated water.
Several injectable inactivated hepatitis A vaccines are available internationally. All provide similar protection from the virus and have comparable side effects.
NOTE: No vaccine is licensed for children younger than 1 year of age.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.