Coping with Chondromalacia

Chondromalacia is a Greek term meaning cartilage softening. More
common among active adolescents and young adults it is associated with the
softening and fibrillation of articular surface of the patella. The basic
disorder is to a major extent caused by mechanical overload of patellfemoral
joint.
Before starting on the detail causes, symptoms and management of this condition
it is essential to understand terms as cartilage, bone, the difference between
them, patella and so on.
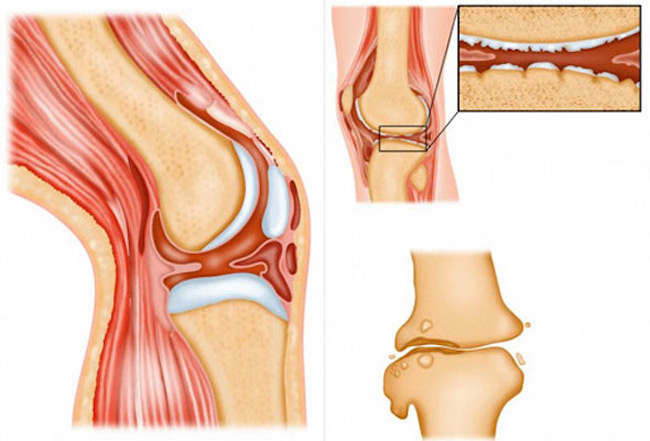
What is a cartilage?
Cartilage is the material that covers the ends of the bones of any joint.
This white, shiny material has a rubbery consistency and is smooth than a state
of ice. The function of articular cartilage is to absorb shock and provide an
extremely smooth bearing surface to facilitate motion. There is articular
cartilage essentially everywhere that two bony surfaces move against one
another, or articulate. In the knee, the cartilage covers the ends of the femur
( large bone of the thigh), the top of the tibia (large bone of the lower leg)
and the back of the patella (fourth bone of the knee joint.), or kneecap. This
material is about 1/4 of an inch thick in most large joints.
Our bones are not very flexible. They aren't supposed to bend. The places where
two bones come together are called joints. Cartilage protects these bones from
rubbing together and causing a lot of pain.
There are three major types of cartilage in the body: 1) hyaline cartilage, 2)
fibrocartilage, and 3) elastic cartilage. Fibrocartilage is permanently present
in form of meniscus of the knee.
How does the cartilage get its nutrition
Cartilage is totally avascular i.e. it has no blood supply like other organs.
Dependent on hormonal and nutritional factors:
-
Nutrition of cartilage comes from underlying canncellous bone by
diffusion.
-
The viscous lubricant material called synovial fluid (a clear,
viscous, pale yellow fluid which fills the synovial cavity). The main
function of the synovial fluid is lubrication and nourishment of articular
cartilage. In a condition like Chondromalacia the quality of this fluid
detoriates due to number of reasons.
-
Vitamin C-The RDA for vitamin C is 60 mg/day. High doses are
often recommended for antioxidant protection. Many experts recommend as much
as 500 to 1,000 mg daily. Fruits and vegetables in the diet guarantee a good
dose of vitamin C. When women think of vitamin C, they think of oranges. But
there are many other great sources such as other citrus fruits, dark green
vegetables, cantaloupes, strawberries, peppers, tomatoes, papayas, and
mangos. A single serving of any of these provides more than 30 milligrams of
vitamin C.
Bone
Vs Cartilage
Cartilage and bone are considered connective tissues. These tissues contain
various amounts and types of matrix, fibers and cells.
|
Variables |
Cartilage |
Bone |
||||||||||||
|
components |
no inorganic substance |
organic substance |
||||||||||||
|
flexibility |
high tensile
strength |
harder |
||||||||||||
|
nutrition
and |
diffusion |
canaliculi-Haversian
system |
||||||||||||
|
mechanism
of |
interstitial and |
appositional growth
only, |
What
is Malacia?
Malacia is the pathological softening of an organ or tissue, such as bone.
Medically, the kneecap is known as the patella and the thigh bone is called the
femur. The knee joint is composed of three bones - the femur (or thigh bone),
the tibia (or shin bone), and the patella (or kneecap). The parts of the knee
joint are subdivided into the tibio-femoral joint which refers to the joint
space between the tibia and the femur; and the patello-femoral joint which is
the joint space between the patella and the femur. Both of these joints (patello-femoral
and tibio-femoral) form the knee joint.
Chondromalacia
Chondromalacia literally means "softening of the cartilage", and Patellae
means "the knee-cap". So Chondromalacia patellae means "softening of the
articular cartilage of the knee-cap." The articular cartilage is the
cartilage lining under the knee-cap that articulates with the knee joint. Under
normal circumstances, it is smooth and shiny, so that it glides smoothly along
the articular groove of the femur as the knee bends. When it "softens", it may
break down, causing irregularities along the undersurface of the patella.
The injury is common among girls aged 10 - 20 years. Correct rehabilitation is
essential for this injury along with taping. Do not ignore this injury because
if it gets very bad it is extremely difficult to treat because of increased
tendency for knouch knee .
It can also happen in the older age-group (in the 40�s and beyond) when the
articular cartilage breaks down as part of the wear-and-tear process that occurs
with the rest of the body. The patella cartilage is one of the earliest places
where cartilage breakdown occurs, and is slowly progressive, leading to
degenerative arthritis (osteoarthritis) in the knee joint.

How is it caused
This can be caused by :
- Recurrent dislocation of the patella (knee cap). In a normal knee, the oblique quadricep muscles insert into the tibia (shine bone) resulting in a valgus angle opening on the lateral side. The supplement to this is the quadricep or Q-angle which in normal cases is 15-20 degree. Continuous exaggeration of the Q-angle leads to dislocation of the patella (knee cap).
-
A muscle imbalance because of weak mid quadriceps muscle (vastus
medialis) and strong hamstring.
-
Postural abnormalities such as pes valgus (flat foot) and
internal rotation of tibia (shine bone).
-
Ischaemia: occurs in muscles when excessive activity may lead to
demands on blood supply which cannot be met.
-
Lack of normal stress, during periods of immobilization.
-
Prolonged repeated stress - which might increase due to increased
load (deformities that might affect the lever system of the joint) or
because of decreased contact area (joint instability).
-
Genetically weak Cartilage.
Symptoms of Chondromalacia
The most frequent symptom of chondromalacia is a dull pain around or under the
kneecap that worsens when walking down stairs or hills. Occasionally the person
may carry a history or injury or recurrent displacement. The symptoms may get
aggravated when climbing stairs or during other activities when the knee bears
weight as it is straightened. The disorder is common in runners and is also seen
in skiers, cyclists, and soccer players.
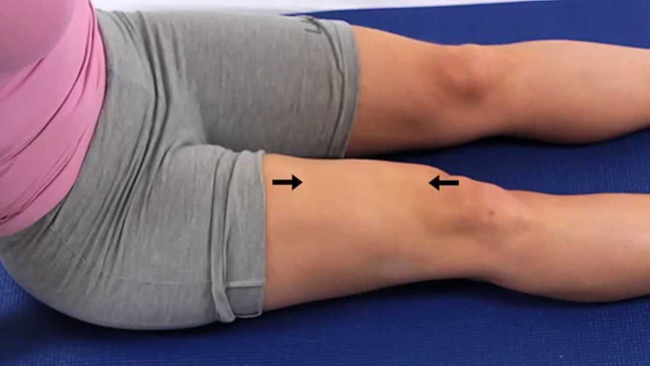
Other signs include:
- Quadricep Wasting
- Fluid in the knee
- Tenderness under the edge of patellae.
- Crepitus on moving the knee.
Call for immediate action:
- Apply RICE (Rest, ice compression and elevation) to the injured knee. This will help reduce swelling.
- Rest until there is no pain (this is very important).
- Use a knee support or heat retainer (with a hole).
-
See a sports injury professional who can advise on treatment and
rehabilitation.
Diagnosis of Chondromalacia
An x-ray usually help the doctor make a diagnosis of chondromalacia. These are
taken at in such a fashion that the relationship of the patella to the femur may
be better identified to allow identification of tracking abnormalities. Although
arthroscopy can confirm the diagnosis of chondromalacia, it is not performed
unless the condition requires extensive treatment.
Aim of the treatment rendered:
For the teenager with chondromalacia, the objective of treatment is to
restore normal patella alignment with the help of exercises. The only way to
alter knee damage is by performing surgery, and sometimes that is required.
However, in most cases, exercises with or without formal physical therapy is all
that is needed to correct the problem. The exercises prescribed should
concentrate on strengthening the vastus medialis obliquus (VMO),
responsible for stabilizing the patella. Once that strengthens, and muscle
balance is restored, the pain improves. In some cases, if the pain persists,
your physician may prescribe physical therapy. The therapist will work at
stretching the vastus lateralis, as well as strengthening the Quadriceps muscle
and Hamstring muscles, using manual and electrical techniques. Occasionally the
therapist may employ a technique called "patella taping" to keep the
patella from tracking laterally.
How Is Chondromalacia Treated
Conservative Management: involves bringing about adjustments in stressful
activities and physiotherapy. Exercises prescribed should be specifically
directed towards strengthening of medial quadriceps so as to counterbalance the
tendency to lateral tilting of the patella.
Your medical professional will give you rehabilitation exercises to carry
out which will help to develop this muscle. For example:
-
Quadriceps contraction: Sit on the floor with your legs fully
extended out in front of you. Place your fingers on top of your vastus
medialis muscles (small bulge of muscle located above the knee, on the inner
side of the thigh). Tighten the thigh muscles, which straightens your knee
for a count of 5. If your vastus medialis is weak, you will feel the muscle
relaxing voluntarily after a few seconds. Each time you do this exercise,
try to maintain the tightness in this muscle. Repeat this exercise 10 times,
on three separate occasions throughout the day. Extension lag is a sign of
quadricep weakness.
This is only one example of a rehabilitation exercise, there are numerous others and your physiotherapist will be able to advise you depending on your specific situation. Once you have addressed this weakness and developed the muscle again - which can take some time - you can begin to exercise normally, but not before then, or you may never fully recover! Activities which you may consider carrying out if YOU MUST, prior to recovery, are those which include full extension (straightening) of the knee, for example: - Front crawl in swimming (not breast stroke).
- Cycling with the saddle adjusted so that you can achieve full extension of the leg, get out of the saddle going up hill.
- Running on flat ground.
Other treatment options:
-
Perform low-impact exercises that strengthen muscles,
particularly the inner part of the quadriceps, without injuring joints to
correct the Q-angle. Swimming, riding a stationary bicycle, and using a
cross-country ski machine are acceptable as long as the knee is not bent
more than 90 degrees.
-
Electrical stimulation may also be used to strengthen the
muscles.
-
If these treatments fail to improve the condition for about 6 months and
the patient is genuinely incapacitated, the physician may perform surgery
to improve patella alignment and reduce patellofemoral pressure.
-
Chondroplasty: or shaving of patella articular surface is
performed arthroscopically (through a telescope making a Key Hole Surgery)
using a powerful tool. Soft and fibrillated cartilage is removed in severe
cases. The operation should be followed by lavage and can be combined with
any of the realignment procedures.
What can be expected after treatment?
Most patients do well with treatment. It is important that you keep up with
the Quadriceps exercises on an indefinite basis. It takes only 5 minutes twice a
day, and is a worthwhile long-term investment for your knees. Also, make sure
you stretch adequately and warm up before sports.
Preventing Chondromalacia
The best way to minimize the chances of developing chondromalacia patellae is to reduce weight (if you are overweight), maintain proper posture, learn to step up with knees as close as possible with ankle under the knee in one line, warm-up and stretch out before sports, especially your quadriceps and hamstrings. If possible, vary your sports. For example, alternate running with swimming with bicycling. Avoid squatting, kneeling, stairs and hill running if you can. In addition there are some exercises that are helpful in preventing and helping the symptoms of anterior knee pain. These exercises should be done regularly, twice a day. If symptoms are already present, it will take about 6 weeks before you get the benefit of the exercise. So, the key is to be consistent, and persistent.
