- The Breast and Breast Cancer
- Types of Breast Cancer
- The importance of Early Life in Breast Cancer Risk
- Risk Factors associated with breast cancer
- Symptoms associated with Breast Cancer
- Detecting Breast Cancer
- Grading of breast cancer
- Treatment Options for Breast Cancer
- Things to Consider During and After Treatment
- Disease Management
- Reducing Your Risk of Breast Cancer
- Breast Cancer & Pregnancy
Cancer is a frightening word surrounded by fears and myths. One of the greatest fears expressed by almost all newly diagnosed cancer patients is: `Am I going to die?’
Approximately 180, 000 American women are newly diagnosed with breast cancer disease each year, and it is the leading killer of women in midlife (ages forty to fifty– five) . The only cancer that kills more women overall is lung cancer , but breast cancer is actually responsible for more years of life lost because it generally afflicts younger women. On top of the physical health problems, breast cancer can also exert a large emotional and psychological toll, because it affects a part of the body that many women associate directly with either femininity. Surveys have consistently found that women perceive cancer to be their greatest health threat.
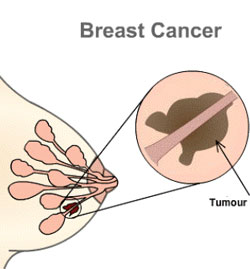
In breast cancer, cells in the breast divide and grow at an abnormal rate, clump together, and from a malignant (cancerous) tumor. There are two main types of breast cancer.
- Invasive Ductal Carcinoma (IDC)- This is a cancer starts in a milk passage, or duct, of the breast, has broken through the wall of the duct, and invaded the fatty tissue of the breast. At this point, it can metastasize, or spread to other parts of the body through the lymphatic system (The tissues and organs that produce, store, and carry white blood cells that fight infections and other diseases. This system includes the bone marrow, spleen, thymus, lymph nodes, and lymphatic vessels (a network of thin tubes that carry lymph and white blood cells). ) and bloodstream. About 80% of invasive breast cancers are infiltrating ductal carcinomas.
- Invasive Lobular Carcinoma (ILC)- Infiltrating lobular carcinoma starts in the milk-producing glands, or lobules. Similar to IDC, it also can spread (metastasize) to other parts of the body. About 10% of invasive breast cancers are ILCs. Invasive lobular carcinoma may be harder to detect by mammography than invasive ductal carcinoma. Stage 1 tumours: these measure less than two centimeters. The lymph glands in the armpit are not affected and there are no signs that the cancer has spread elsewhere in the body.
Stage 2 tumours: these measure between two and five centimeters, or the lymph glands in the armpit are affected, or both. However, there are no signs that the cancer has spread further.
Stage 3 tumours: these are larger than five centimeters and may be attached to surrounding structures such as the muscle or skin. The lymph glands are usually affected, but there are no signs that the cancer has spread beyond the breast or the lymph glands in the armpit.
Stage 4 tumours: these are of any size, but the lymph glands are usually affected and the cancer has spread to other parts of the body. This is secondary breast cancer. - Ductal Carcinoma in situ (DCIS) – This is also called a noninvasive breast cancer, where there are abnormal cells in the breast, but they are not cancerous and have not spread to other nearby tissue. In situ means “in place”. Still, carcinoma in situ is a sign that breast cancer may develop at a latter time. The main categories of carcinoma in situ are ductal carcinoma in situ (DCIS) –where the abnormal cells originate in the milk ducts – and lobular carcinoma in situ (LCIS) – where the abnormal cells originate in the lobules. A mammogram is the best way to find DCIS early.
The best chance of surviving breast cancer comes from the early detection of carcinoma tumors through regular clinical breast exams and mammograms. Reducing the risk of the disease ever occurring, however, should be every woman’s goal.
The importance of Early Life in Breast Cancer Risk
The National Cancer Institute and U.S. Department of Health and Human Services recommend that women in their forties and older have mammograms every one to two years. A complete early detection plan also includes monthly breast self-exams and clinical breast examinations by a trained medical professional. |
Ideally the prevention of breast cancer would start in youth and young adulthood, as this period has been found to be extremely important in determining a woman’s risk of developing breast cancer later in life. Breast tissue during this time (from youth up until a woman gives birth to her first child) appears to be more susceptible to elements that can cause cells to subsequently become cancerous. Exposure to radiation is a good example. The risk for adult breast cancer is very high for a girl under ten exposed to high dose of radiation , moderate for a teenager, and small for a young adult.
Risk Factors associated with breast cancer
To many woman it would seem that just about everything affects the risk of developing breast cancer. While this is not the case, the scientific community has come a long way in identifying many factors that increase the risk of the disease. These factors can range from history to lifestyle to reproductive variables.
Although there are few factors that substantially increase a woman’s risk of breast cancer, most individually elevate or lower risk by only a small amount. Risk factors have been categorized as ones over which:
- a woman has control (such as alcohol consumption and use of postmenopausal hormones) and
- a woman doesn’t have control (such as breast cancer in an immediate family member and age at menarche). By knowing how each of these factors affects her risk, a woman can take appropriate steps to try to protect herself from the disease.
Factors that cannot be controlled :
These are a number of factors beyond a woman’s control that affect her risk of developing breast cancer. Understanding these may lead a woman to be more vigilant about those factors under her control and, if necessary, seek more frequent check ups or screening tests.
In a group of I00 women who are fifty years old, 9 will develop breast cancer before they reach the age of eighty. The I in 8 numbers that many women recognize is the lifetime risk of breast cancer. This means that for all adult women, I in 8 (or approximately I 2 percent) is at risk of developing breast cancer in her lifetime. While a I2 percent lifetime risk is high for a serious disease like breast cancer, the lifetime risk of coronary heart disease is much higher (about 32 percent), and both coronary heart disease and lung cancer kill more women overall.
It should come as no surprise that family is linked to the risk of breast caner. Most people realize that the risk of many diseases are associated with the experiences of their parents an siblings.
The age at which the mother was diagnosed, however, influenced the level of risk as well .The younger the mother was when she was diagnosed with the disease, the higher her daughter‘s risk of developing breast cancer. A woman whose mother was diagnosed before age forty has a large increase in risk, while a woman whose mother was diagnosed after age seventy has only a moderate increase in risk.
Family members usually have very similar lifestyles and therefore may have similar “environmental “risk factors for breast cancer – such as weight, activity level, and alcohol intake. While this may account for the increased risk of breast cancer experienced by some families, in some cases genetics likely plays a large role.
The term benign breast disease is often used to describe a wide range of non-cancerous conditions that can affect the breast. Two specific types of benign breast disease – hyperplasia and radical scars – increase the risk of developing breast cancer. Other benign breast conditions, such as cysts and fibroadenomas, do not appear to influence risk.
The density of a woman’s breast has been shown in many studies to be strongly related to the risk of breast cancer. Breast density is most often assessed by mammogram and depends on the proportion of fat and tissue that make up a woman’s breasts. When the X-rays used in a mammogram take an image of the breast, fat appear dark and tissue appears light. Breasts with a high density have a relatively high proportion of tissue and low proportion of fat. Breasts with a low density have a relatively low proportion of tissues and high proportion of fat.
Of note, one very large cohort study found that women with the most dense breasts had approximately 5 times the risk of breast cancer compared to women with the least dense breasts. And as breast density increased, so did the risk of the disease.
Radiation Exposure in Childhood or Adolescence
Exposure to high doses of radiation to the chest in childhood or adolescence has been consistently linked to an increased risk of breast cancer in later adulthood. Studies have found that women who were exposed in their youth to atomic bomb blasts (in Hiroshima or Nagasaki, Japan) or radiation therapy for disorders like Hodgkin’s disease or tuberculosis had 2 to 4 times the risk of breast cancer compared to women who were not exposed to such radiation. The greatest risk is generally in those women who were very young when exposed, and the risk decreases as the age at the exposure increases. Women over forty who have been exposed to high doses of radiation to the chest have only a small increase in risk.
Just as family history can affect the risk of breast cancer, so can a personal history of cancer. Women who have been previously diagnosed with cancer in one breast are at increased risk of developing cancer in the other breast.
Having a personal history of lobular carcinoma in situ – which is usually not treated after diagnosis, just closely followed – also increases the risk of cancer. Women with this condition are 7 to 10 times more likely to develop breast cancer than women without the condition.
Not all groups of women in the United States are equally impacted by breast lowest risk of Latina, Asian American Indian women tend to have the lowest risk of breast cancer risk in the United States, and white women tend to have the highest risk – followed closely by Hawaiian American and Africa American can women.
For breast cancer occurring before midlife, however, African American women are at highest risk. This is likely due, at least in large part, to differences in the ages at which white women and African American women first give birth.
Height is generally thought to reflect, at least in part, the quantity and quality of the diet in childhood . Well fed children generally have more rapid, bigger growth spurts than children fed poor diets. This many contribute to breast cancer risk because such rapid growth can increase the chance that the DNA in some breast cells will become permanently damaged , which can lead to cancer later in life .One other possibility is that levels of a hormone called insulin – like growth factor are higher in taller children than in shorter children . In some studies , high levels of insulin – like growth factor have been linked to an increased risk of breast cancer.
Factors You Can Control:
It is important to know how all of the factors related to breast cancer make up a woman’s risk. However, when given a choice, most women would prefer to focus on those things they have control over and can change for the better. These so-called modifiable factors are discussed in this section and range from alcohol intake to use of postmenopausal hormones.
Vitamin A, Carotenoids, and Vegetables. A number of studies have linked a low intake of vitamin A and carotenoids, such as beta – carotene, with an increased risk of breast cancer. Found in high amounts in green and yellow vegetables and certain fruits, vitamin A is important for cell growth, and carotenoids are powerful antioxidants that can help protect cells from the damaging effects of oxygen free radicals in the body.
Dietary Fat: Eating high amounts of total fat in adulthood appears to have little, if any, effect on the risk of developing breast cancer. According to a survey, It was found that women with a high fat diet do not have a greater risk of developing breast cancer .Similarly, women who ate little fat (20 percent or less of total calories) did not have a lower risk of the disease compared to women who ate a moderate amount. This analysis found their neither a high fat diet nor a low fat diet was related to the risk of breast cancer .
High intake of monounsaturated fat (found in olive and canola oil) has been found in some studies to lower the risk of breast cancer.
Estrogen Levels: Many modifiable factors can increase the level of estrogen in the body, and therefore increase the risk of breast cancer. Examples of such factors include gaining substantial weight as an adult; being overweight and physically inactive after menopause ; drinking modest amounts of alcohol ; or postmenopausal hormones.
Overweight and Weight Gain: Being overweight is thought to increase the risk of breast cancer after menopause primarily by increasing levels of the hormone estrogen. Although a woman‘s ovaries stop producing estrogen after menopause, her fat tissue converts estrogen precursors to estrogen. The more weight put on after menopause, the more estrogen that is produced . This relation of weight to hormone levels explains why breast cancer risk in overweight postmenopausal women appears to be more pronounced in those who have never taken postmenopausal hormones. The amount of estrogen contained in postmenopausal hormones far outweighs that produced by the fat tissue in overweight and obese women. Therefore, the full effect of weight on breast cancer risk can become masked when a woman uses postmenopausal hormones. It is not that taking postmenopausal hormones eliminates the risk of breast cancer associated with being overweight; it is that using hormones likely hides the effect of weight on risk.
Body Shape: Body shape also seems to influence the risk of breast cancer in postmenopausal women. Women who are apple – shaped – those who tend to carry extra weight around the waist – seem to be at higher risk of breast cancer than women who are pear – shaped – those who tend to carry extra weight in their hips and thighs. Similar to the results of other studies, we found that postmenopausal women with the largest waist sizes have about a 35 percent greater risk of breast cancer compared to those with the smallest waist sizes. As with overall weight, the full effect of waist sizes on breast cancer risk may be obscured by the use of postmenopausal hormones.
Physical Activity: Numerous studies have examined the relationship between physical activity and breast cancer risk, but results to data have been somewhat inconsistent. This variability in findings likely relates to the different approaches researches use to assess a woman’s level of physical activity, which can be difficult to measure accurately. Postmenopausal women who engage in at least one hour of physical activity a day are I 5 to 20 percent less likely to develop breast cancer than women who are sedentary.
Physical activity may help lower the risk of breast cancer in postmenopausal women by helping curb weight gain, which in turn helps keep estrogen levels in check. In young girls, physical activity may have the added benefit of putting off the age at which a girl first has period, therefore reducing lifetime exposure to estrogen.
Alcohol: Drinking alcohol does not come without accompanying risks especially for women. It has been found that even fewer than 2 drinks per day could increase risk. Compared to women who did not drink, those who drank about half a drink to one drink a day had a small increase in the risk of breast cancer , and those who drank more than one drink a day had a moderate increase in risk.
Postmenopausal Hormones: A large number of U.S. women take postmenopausal hormone therapy to alleviate the short – term symptoms and longer – term health effects of menopause. While such hormones therapy appears to be beneficial in many ways – lowering the risk of osteoporosis and possibly coronary heart disease and colon cancer – it also increase the risk of breast cancer in certain users.
Because postmenopausal hormones that contain only estrogen have been shown to increase the risk of cancer of the uterus, more and women are choosing to take hormones that contain both estrogen and progestin. It was initially thought this combined therapy might reduce the excess risk of breast cancer linked to postmenopausal hormones.
Birth Control Pills: The use of birth control pills moderately increases the risk of breast cancer in those women who are currently using them. Women who are currently taking the pill had a 50 percent increase in risk compared to women who have never used the pill . Women who had used the pill in the past (but were not doing so currently) did not show any increase in breast cancer risk. Moreover, how long a woman had been on the pill did not seem to change the results.
Although the pill seems to slightly increase breast cancer risk in current users, it also has many benefits. In addition to preventing unwanted pregnancy, it lowers the risk of ovaries and endometrial cancers. Also, when women use the pill, it is during a time in life when their absolute risk of breast cancer is low, so even though a 50 percent increase in risk is substantial, it will actually result in only a few extra women developing breast cancer who otherwise would not have. Assessing such individual risk and benefits and the impact they have on a woman’s lifestyle is key to determining whether or not she sue birth control pills
Symptoms associated with Breast Cancer
Possible symptoms of breast cancer include:
- A lump or thickening in or near the breast or in the underarm area.
- A change in the size or shape of the breast.
- Thickening, swelling, distortion, or tenderness of the breast
- Skin irritation or dimpling
- Nipple pain, scaliness, ulceration, or retraction.
- A change in the way the skin of the breast, areola, or nipple looks or feels (for example, warm, swollen, red, or scaly).
- Swelling or lump in armpit.
Breast pain is commonly due to benign conditions and is usually not the first symptom of breast cancer.
Women should talk with their doctor about factors that can increase their chance of getting breast cancer. Women of any age who are at higher risk for developing this disease should ask their doctor when to start and how often to be checked for breast cancer. Breast cancer screening has been shown to decrease the risk of dying from breast cancer.
Women can take an active part in the early detection of breast cancer by:
- Regular scheduled screening (Checking for disease when there are no symptoms) by a doctor,
- Mammograms
- Ultrasonography and
- Clinical breast exams (breast exams performed by health professionals). click here, for breast self-exams.
A screening mammogram is the best tool available for finding breast cancer early, before symptoms appear. A mammogram is a special kind of x-ray. Screening mammograms are used to look for breast changes in women who have no signs of breast cancer. Mammograms can often detect a breast lump before it can be felt. Also, a mammogram can show small deposits of calcium in the breast. Although most calcium deposits are benign, a cluster of very tiny specks of calcium (called microcalcifications – A tiny deposit of calcium in the breast that cannot be felt but can be detected on a mammogram. A cluster of these very small specks of calcium may indicate that cancer is present) may be an early sign of cancer.
If an area of the breast looks suspicious on the screening mammogram, additional (diagnostic) mammograms may be needed. Depending on the results, the doctor may advise the woman to have abiopsy (The removal of cells or tissues for examination under a microscope. When only a sample of tissue is removed, the procedure is called an incisional biopsy or core biopsy. When an entire lump or suspicious area is removed, the procedure is called an excisional biopsy. When a sample of tissue or fluid is removed with a needle, the procedure is called a needle biopsy or fine-needle aspiration).
Although mammograms are the best way to find breast abnormalities early, they do have some limitations. A mammogram may miss some cancers that are present (false negative) or may find things that turn out not to be cancer (false positive). And detecting a tumor early does not guarantee that a woman’s life will be saved. Some fast-growing breast cancers may already have spread to other parts of the body before being detected.
Most doctors recommend that women in their forties and older should have mammograms regularly, every 1 to 2 years.
Colour dropler
Certain types of ultrasound machine show the blood supply to the lump and this may help to distinguish between a cancer and a benign lump. The blood supply shows up as patches of red or blue colour on the scan.
Blood tests
Samples of your blood will be taken to check your general health, the number of cells in your blood (blood count) and to see how well your kidneys and liver are working. Your blood may also be tested to see whether it contains particular chemicals (called markers) which are sometimes produced by cancer cells
Some women perform monthly breast self-exams to check for any changes in their breasts. When doing a breast self-exam, it’s important to remember that each woman’s breasts are different, and that changes can occur because of aging, the menstrual cycle, pregnancy, menopause, or taking birth control pills or other hormones. It is normal for the breasts to feel a little lumpy and uneven. Also, it is common for a woman’s breasts to be swollen and tender right before or during her menstrual period. Women in their forties and older should be aware that a monthly breast self-exam is not a substitute for regularly scheduled screening mammograms and clinical breast exams by a health professional.
Grading refers to the appearance of the cancer cells under the microscope. The grade gives an idea of how quickly the cancer may develop. There are three grades:
- grade 1 (low grade),
- grade 2 (moderate grade) and
- grade 3 (high grade).
Low grade means that the cancer cells look very like the normal cells of the breast. They are usually slowly growing and are less likely to spread. In high grade tumours the cells look very abnormal. They are likely to grow more quickly and are more likely to spread.
Treatment Options for Breast Cancer
Treatment of breast cancer varies according to the nature and extent of the cancer, the opinion of the doctor or doctors and the wishes of the patient. To play an active role in treatment decisions, a patient should gather as much information as he or she can about a particular diagnosis. In some cases the breast is removed completely along with surrounding tissues. This is called a modified radical mastectomy, and for many years it was the only treatment available. Now, in some cases in which the cancer is fairly small and localized — which means it has not spread outside the breast — it is possible to remove only the lump and some of the surrounding tissue. This procedure is sometimes called a “lumpectomy.” Lumpectomies are generally followed by radiation to the breast. Sometimes chemotherapy may also be administered. For both mastectomy and lumpectomy procedures, lymph nodes near the tumor are generally removed as well.
Patients with high risk breast cancer may be offered autologous blood stem cell transplantation with a special treatment called the Stamp V regimen.
Treatment(s) may involve:
- A lumpectomy is a less invasive surgical technique that involves removing thetumor and the lymph nodes (Hundreds of small bean shaped organs (sometimes called glands) located throughout specific area of the body in the lymphatic system. They act as filters to collect and destroy bacteria. Cancer cells that may be moving through the lymphatic system can get trapped in the lymph nodes) under the arm but not the whole breast.
- A mastectomy can be segmental or total. In segmental mastectomy, the surgeon removes the cancer and a larger area of normal breast tissue around it. Total mastectomy is more invasive and is the surgical removal of the breast and the lymph nodes under the arm. Breast reconstruction is often an option at the same time as the mastectomy, or later on. Women considering reconstruction should discuss this with a plastic surgeon before having a mastectomy.
- Breast Conserving Surgery- an operation conducted to remove the breast cancer but not the breast itself. Types of breast-conserving surgery include lumpectomy,quadrantectomy, and segmental mastectomy (removal of the cancer as well as some of the breast tissue around the tumor and the lining over the chest muscles below the tumor). Also called breast-sparing surgery.
- Hormone therapy – Several types of cancer can only grow and spread in the presence of natural chemicals in the body called hormones. Other types of cancer, however, are slowed by specific hormones. The use of treatments that fight cancer by altering the amounts of these hormones in the body is called hormone therapy. This type of therapy is especially useful for treating many cancers of the breast and reproductive system.
- Chemotherapy- Chemotherapy is most often used when a cancer is not isolated in one place but when it has metastasized or spread throughout the body. Chemotherapy is also used to lessen the chances that tumor cells that have spread, but can not be detected, will grow. Chemotherapy is delivered to every tissue in the body by the bloodstream. These drugs fight cancer by interfering with the metabolism or growth process of cancer cells, eventually causing the cells to die. For many cancers, combinations of chemotherapy medicines are given because they are more effective given together, than alone.
Chemotherapy regimens can be given in many ways, such as:
- Oral (by mouth)
- Topical (on top of the skin as a cream or lotion)
- Intravenous (into a vein or IV)
- Intraperitoneal (into the abdominal cavity or IP)
- Intralesional (into the tumor)
- Radiation therapyy- Radiation is useful in treating many types of cancer. It is often used when the cancer is in one, or a small number of places in the body. Radiation therapy uses beams of high-energy waves or streams of particles including X-rays, gamma rays, andelectrons to destroy cancer cells. Like chemotherapy, radiation therapy halts the growth and division of cancer cells and causes them to die.
Two main types of radiation are used, external beam radiation and internal radiation or brachytherapy. External beam radiation focuses on the tumor from outside of the body. It is much like getting a diagnostic X-ray, but for a longer time. Before treatments start, imaging studies such asMRIs, CT scans, or plain X-rays are done to find the exact location of the tumor. The radiation team will then make some ink marks on the skin, that they will later use as a guide, to focus the radiation in the right area. Each treatment lasts only a few minutes and is painless. Brachytherapy uses small radioactive pellets or “seeds” that are placed near the tumor. Treatments are often combined with external beam radiation, which is given at a lower dose than it normally would be if used by itself.
5. Biological therapy is a treatment designed to enhance the body’s natural defenses against cancer. For example, Herceptin® (trastuzumab) is a monoclonal antibody (A laboratory-produced substance that can locate and bind to cancer cells wherever they are in the body. Many monoclonal antibodies are used in cancer detection or therapy; each one recognizes a different protein on certain cancer cells. Monoclonal antibodies can be used alone, or they can be used to deliver drugs, toxins, or radioactive material directly to a tumor.) that targets breast cancer cells that have too much of a protein known as human epidermal growth factor receptor-2 (HER-2). By blocking HER-2, Herceptin slows or stops the growth of these cells. Herceptin may be given by itself or along with chemotherapy.
A woman’s treatment options depend on a number of factors. These factors include her age and menopausal status; her general health; the size and location of the tumor and the stagee (The extent of a cancer within the body. If the cancer has spread, the stage describes how far it has spread from the original site to other parts of the body.) of the cancer; the results of lab tests; and the size of her breast. Often, two or more methods are used in combination. In most cases a lumpectomy is followed by several weeks of :
- Radiation, then chemotherapy, or
- Hormone therapy, then radiation.
Things to Consider During and After Treatment
During and after your treatment for breast cancer you may be able to speed up your recovery and improve your quality of life by:
- Taking an active role in the treatment process. Learn about the benefits and risks of each of your treatment options, and ask questions of your cancer care team if there is anything you do not understand. Learn about and look out for side effects of treatment, and report these right away to members of your cancer care team so they can take steps to ease them and shorten their duration.
Remember that your body is as unique as your personality and your fingerprints. Although understanding your cancer’s stage and learning about your treatment options can help predict what health problems you may face, no one can say for sure how you will respond to cancer or its treatment.
You may have special strengths such as a history of excellent nutrition and physical activity, a strong family support system, or a deep faith, and these strengths may make a difference in how you respond to cancer. There are also experienced professionals in mental health services, social work services, and pastoral services who may assist you in coping with your illness.
- Opting for a healthy lifestyle: You can help in your own recovery from cancer by making healthy lifestyle choices. If you use tobacco, stop now. Quitting will improve your overall health and the full return of the sense of smell may help you enjoy a healthy diet during recovery. If you use alcohol, limit how much you drink. Have no more than 1 or 2 drinks per day. Good nutrition can help you get better after treatment. Eat a nutritious and balanced diet, with plenty of fruits, vegetables, and whole grain foods.
- Rest: If you are being treated for cancer, be aware of the battle that is going on in your body. Radiation therapy and chemotherapy add to the fatigue caused by the disease itself. Give your body the rest it needs so that you will feel better as time goes on. Exercise once you feel rested enough. Ask your cancer care team whether your cancer or its treatments might limit your exercise program or other activities.
- It is important that you consider your emotional, psychological, and spiritual health along with the physical aspects of your recovery from cancer.
- Side effects of treatment: A woman’s choice of treatment will likely be influenced by her age, the image she has of herself and her body, her hopes and fears, and her stage in life. For example, many women select breast-conserving surgery with radiation therapy over a mastectomy for body image reasons. On the other hand, some women who choose mastectomy may want the affected area removed, regardless of the effect on their body image, and others may be more concerned about the side effects of radiation therapy than body image. Other issues that concern women include loss of hair from chemotherapy and skin changes of the breast from radiation therapy. In addition to these body changes, women may also be concerned about the outcome of their treatment. These are all factors that affect how a woman will make decisions about her treatment, how she views herself, and how she feels about her treatment.
- Concerns about sexuality are often very worrisome to a woman with breast cancer. Some treatments for breast cancer can change a woman’s hormone levels and may have a negative impact on sexual interest and/or response. A diagnosis of breast cancer when a woman is in her 20s or 30s is especially difficult because choosing a partner and childbearing are often very important during this period. Relationship issues are also important because the diagnosis can be very distressing for the partner, as well as the patient. Partners are usually concerned about how to express their love physically and emotionally during and after treatment.
A cancer diagnosis and its treatment holds a major life challenge, with an impact on you and everyone who cares for you.
Women who have undergone treatment for breast cancer should be reassured that their quality of life, once treatment has been completed, will be normal. |
Defining an Exercise Regime: Exercise for the patient who has had breast surgery is important to the entire body and mind. But specifically, it will speed up recovery from the effects of surgery. Any surgery on the breast, whether a lumpectomy, removal of nodes under the arm, or a mastectomy, will cause soreness and discomfort. While the immediate healing process is occurring, exercise of the area (including the arm or shoulder) should be at the physician’s direction. Once healing is progressing, exercise of the arm and shoulder is very important. The shoulder joint and the muscles will tighten. If they are not used, their function will be limited. This will lead to discomfort as well as unnecessary loss of use.
The Reach to Recovery Program of the American Cancer Society has an excellent manual which gives specific exercises to assure a full range of motion. These include reaching, pulling, and rotating the arm behind the back to further stretch the shoulder joint. These exercises must be done on a regular schedule to assure full use of the arm and shoulder. Programs using aerobics and swimming can also accomplish the same results but should be done under the direction of a knowledgeable instructor. You can also try innovative forms of exercise: squeezing a ball with the hand, touching a board with the feet, weight lifting with books.
Becoming physically fit is an excellent way to enhance your capacity to cope with the diagnosis and treatment of cancer. By striving for your most realistic level of physical fitness, you become can get fit.
In the study, published in the American Journal of Epidemiology(10 February, 2003), researchers from the German Cancer Research Centre in Heidelberg said: “We found decreasing risks with increasing cycling activity levels. They added: “For cycling, we found a significant protective effect, and sports appeared to have some protective effect among otherwise less active women.” .It could be that cycling improves your immune system.
Nutritional Needs: The nutrient needs of a cancer patient vary from person to person. Your doctor, nurses, and dietitians can help you to identify your nutrition goals and plan strategies to help you meet them. You need to eat a variety of foods that will provide the nutrients you need to maintain your health while fighting cancer. These nutrients include protein, carbohydrates, fat, water, vitamins, and minerals.
Eating a balanced diet can be challenging when you are receiving cancer treatment, particularly if treatment side effects persist for long periods of time. Make use of the American Cancer Society Nutritional Guidelines to plan what to eat each day.
- Following surgery, chemotherapy, and radiation therapy, additional protein is usually needed to heal tissues and to help prevent infection. Eat high-protein foods first, when your appetite is strongest. Good sources of protein include lean meat, fish, poultry, dairy products, nuts, dried beans, peas and lentils, and soy foods.
- Eat five or more servings of a variety of vegetables and fruits each day.
- Choose whole grains in preference to processed (refined) grains and sugars.
- Limit consumption of red meats, especially those high in fat and processed.
- Choose foods that help you maintain a healthful weight.
- Eat several small meals a day instead of three large meals.
- Take interest in food by trying new recipes and products.
- Drink beverages between meals instead of with meals.
- Aim for eight glasses glasses of liquid each day.
In case of weight gain:
- Select healthy foods including variety of vegetables, fruits, whole grains, and beans.
- Eat only when you’re hungry. Eating to comfort feeling of stress, fear or depression will not alleviate those emotions.
- Pay attention to your portion-sizes.
Click here, for Suggestions For Healthy Eating After Cancer
Spiritual Healing: Spirituality is defined as caring for the “soul”, and not every person believes in spirituality, but to those who believe, faith and prayer have been shown to have a positive affect. There is scientific research to suggest that it is possible to influence health with the mind. In fact, mind/body interventions have become more popular among mainstream medicine. Therapies like Tai Chi, Meditation involve using the mind and/or movements of the body as a source of healing. Meditation can be done alone, or can be lead in a group. Meditation is excellent for stress reduction. Similar to meditation is guided visualization, which uses mental imagery to let go of negative energy, and create positive images. Visualization can be done alone, or can be lead by a professional or an audiotape.
For more and latest advances in Breast Cancer treatment, click here
Emotional Health: The most common sexual side effects stem from damage to a woman’s feelings of attractiveness. In our culture, we are taught to view breasts as a basic part of beauty and femininity. If her breast has been removed, a woman may be insecure about whether her partner will accept her and find her sexually pleasing. Therefore, it is important that your focus on tests and treatments does not prevent you from considering your emotional state.
- A woman’s choice of treatment will likely be influenced by her age, the image she has of herself and her body, and her hopes and fears. For example, some women may select breast-conserving surgery with radiation therapy over a mastectomy for cosmetic and body image reasons. On the other hand, some women who choose mastectomy may want the affected area removed, regardless of the effect on their body image. They may be more concerned about the effects of radiation therapy than body image. Your doctor will tell you when you have healed enough to be fitted for a permanent breast form or prosthesis.
- Other issues that women worry about include hair loss from chemotherapy and skin changes of the breast from radiation therapy. In addition to these body changes, women may also be dealing with concerns about the outcome of their treatment.
- It is important to remember that some treatments for breast cancer, such as chemotherapy, can change a woman’s hormone levels and may negatively affect sexual interest and/or response. A diagnosis of breast cancer when a woman is in her 20s or 30s is especially difficult because choosing a partner and childbearing are often very important during this period.
- Relationship issues are also important because the diagnosis can be very distressing for the partner, as well as the patient. Partners are usually concerned about how to express their love physically and emotionally after treatment, especially surgery. Breast surgery will not affect your physical ability to have sex, the accompanying strong emotions may affect your sexual feelings for a while. Women often need to feel relatively happy with their bodies to have a fulfilling sex life. Fear that a partner — even a long-standing one — may be put off by the result of the surgery can make women fearful of the moment they allow someone to see or touch their body. There is no right or wrong time to take this step. When you do it, and the way you do it, depend entirely upon your own feelings and your relationships.
Suggestions that may help a woman adjust to changes in her body image include looking at and touching herself; seeking the support of others, preferably before surgery; involving her partner as soon as possible after surgery; and openly communicating feelings, needs, and wants created by her changed image.
This section has dealt mainly, and briefly, with the immediate emotional impact of breast cancer surgery. This is not meant to imply that in a few months you should feel fine and have fully accepted the changes to your body. The emotional roller-coaster often lasts longer: you may find all your anxieties returning each time you have to go for a follow-up appointment. New situations may bring fears, anger and insecurities flooding back; women without a partner, for example, may be particularly anxious if and when the time comes to get sexually involved with someone.
Reducing Your Risk of Breast Cancer
There are many things that can be done that may help reduce your risk of breast cancer:
- Reduce your dietary fats. High levels of dietary fat have been linked with a higher incidence of breast and colon cancer. Limit red meat to two or three servings per week and choose low-fat dairy products. Fat intake should be no more than 30% of your total daily food intake.
- Increase fiber intake. A diet higher in fiber is automatically lower in fat. Increase your fiber intake by:
1. Eating high-fiber cereal for breakfast every day
2. Snacking on fresh fruits and vegetables
3. Using whole grain breads and brown rice
4. Including legumes, beans and whole grains in your soups and salads - Eat a well-balanced diet. Be sure to include foods that have vitamins A, C and E and Selenium, all of which have been found to possibly offer some protection against cancer. Don’t smoke, and drink alcohol only in moderation.
Decrease caffeine if bothered by lumpy, tender breasts with symptoms becoming worse just before your period. Caffeine is found in coffee, tea, colas, chocolate and some medicines. - Decrease weight, especially if you are 20 pounds or more overweight. Obese women are at an increased risk for having both breast and uterine cancer.
- Learn to cope with stress in your life and reduce its harmful effects. Coping mechanisms include exercise, relaxation, friendships and hobbies. Researchers now believe that difficulty handling stress may lead to an increase in health problems, including cancer.
- Women at high risk should talk with their doctor about other things that can be done to reduce their risk, such as: getting their first mammogram before age 40, mastectomy and taking Tamoxifen or Raloxifene.
Pregnancy usually is safe for women who are free of cancer and not undergoing treatment.
Several studies now have shown that getting pregnant after successful treatment for breast cancer doesn’t increase the risk of a cancer recurrence or death, at least in women who had small tumors and negative lymph nodes. For example, one study from the University of Washington paired up 53 women who became pregnant after a breast cancer diagnosis with other women who had similar breast cancer histories but who didn’t become pregnant later. The researchers found no evidence that getting pregnant had an adverse effect on survival.
Many doctors still suggest that women wait two years after diagnosis with breast cancer before trying to have a baby. The two-year period is used because most recurrences happen during that time, which might affect a woman’s decision to become a mother.
